Grade II leiomyosarcoma of left knee with pleomorphic differentiation:
Christine Talbot. SRN. MLD.DLT.
History:
October 2021
Mr W made a routine visit to his GP for a blood pressure check as he fainted at home, he thought it was medication related but nothing untoward was found.
Many years back Mr W had had a very serious horse riding accident on top of high cliffs, he thinks the horse stumbled, rolled on top of him and levered back up on his body crushing his chest, fracturing ribs and perforating his lung. His life was saved as a Naval helicopter was passing overhead at the time of the incident and airlifted him to a major trauma unit.
Recently he had complained about a painful bump on his left knee which could have related back to the riding accident, his GP felt an ultrasound was advisable to allay any concerns as the discomfort had not resolved.
November 2021
Ultrasound, was inconclusive and indicated further investigations were necessary but it was thought there was a tumour of the left knee.
December 2021
Mr W was referred to a general surgeon.
January 2022
Mr W was referred on to a specialist oncoplastic consultant in breast and soft tissue surgery.
CT and MRI confirmed a Sarcoma of the left knee.
Late January 2022
Referred to a sarcoma specialist at The Royal Marsden.
February 2022
Treatment plan:- twenty-five sessions of radiotherapy at a local hospital prior to planned resection. Surgery for early May.
10.05.2022
Mr W admitted for surgery to The Royal Marsden two weeks prior to his 87th birthday.
07.06.2022
Mr W discharged home from The Royal Marsden with crutches.
10.05.22 Operation:
Resection of sarcoma, left vastus intermedius/medialis.
Histology:
- Pleomorphic single cell sarcoma with bizarre cells and tumour necrosis.
- Excision Margins, crucial cranial margin-muscle without tumour.
- Lymphovascular invasion, not detected.
- Tumour maximum, dimension 131mm superficial to deep.
- Pathology staging, pT3 N0 G2.
Post operative complications:
Chest infection within twenty-four hours, treated with antibiotics.
Wound infection with associated cellulitis. IV antibiotics (guided by drain cultures), a subsequent drain was inserted under ultrasound to drain the collection in the left distal thigh.
Infected with Covid 19 as an inpatient but made a good recovery.
17.06.22 Lymphatic treatment and rehabilitation:
Manual lymph drainage commenced three days post discharge.
On my first visit Mr W was deeply traumatised, frightened and in a great deal of pain, his five weeks in hospital had been very challenging, his whole experience from diagnosis to discharge had left him in a state of disbelief, shock and extreme negativity.
Mr W was fortunate to have a wonderfully supportive wife but she has significant health problems and would not have been able to manage the immediate requirements of aftercare from major surgery. Initially district nurses and HCA’s were attending to help with getting up and going to bed and checking his wound. At times they were alarmed by the induration and erythema around the operative site, this appearance is a familiar effect of pre operative radiotherapy, a prolonged deep wound infection and cellulitis causing a haemosiderin stain. The knee area was not unduly warm and Mr W was nonfebrile.
Physiotherapy commenced, this was another hurdle for Mr W, he was very reluctant to move and spent hours sitting out watching the television, a familiar pattern pre-diagnosis. Gradually he gained some mobility with a Zimmer and would walk around indoors. Mr W’s mobility gained in confidence whereby he felt able to graduate to a walking stick, however whilst home alone he fell down a step in the garden hurting his back and shoulder, his confidence greatly regressed even though his left knee was undamaged.
NHS physiotherapy was for a limited period so Mr W graduated on to a six week GP referral to a local gym for fitness rehabilitation. With much reluctance and at times dogged opposition Mr W attended these sessions with positive improvement. His main and only aim whilst in hospital was to be able to return home and walk his beautiful dog Marley. With great encouragement, physical instruction and lymphatic drainage Mr W was able to walk out with Marley after three months of major surgery, within six months he was again driving, undertaking small tasks in the garden and local shopping.
17.06.22 Method of Treatment.
Mr W was very traumatised overall, made worse following a late evening discharge from hospital with a long, uncomfortable and painful journey home in an ambulance. Both he and his wife felt very isolated, frightened and completely out of their depth in how to manage.
They required much reassurance and support in the early weeks.
Advice was given on the importance of taking regular pain medication particularly at night and the use of an ice pack to lessen pain and heat around the left knee. Early ambulation on a repeated regular basis throughout the day was advised to alleviate stiffness to encourage the limb to re-establish near normal function and increase muscle tone. Mr W was shown hamstring curls to flex and extend the knee as this action would pump lymph and vascular flow through the operation site. A stretchy band was introduced to place around the foot for flexion and extension to strengthen ankle mobility and pump the calf.
On the first visit only the Quantum Wave Laser was used as Mr W was too anxious. Within that hour great benefit was seen and felt which from there on allowed the combined use of Deep Oscillation, laser therapy and the Magcell, (a powerful magnet to aid blood flow) Later the Rolly was introduced to help push fluid to the root of the limb and to relieve any congestion around the knee which he could do himself.
Each weekly visit all advice had to be repeated as Mr W was reluctant to accept any progress, but he was amazed at how quickly his raised scar line was disappearing, how much more movement he had in his knee and his decrease in knee pain, plus any discomfort and fluid engorgement in the thigh reduced at each appointment.
Mr W has regular follow up appointments at his local hospital, he has had chest x-rays to ensure there is no spread, nor have the scans shown any signs of recurrence at the knee.
All three consultants and Mr W’s GP are amazed he has in a short space of time made a remarkable and most unexpected recovery considering his age, the type of cancer he had and his post operative complications. Their acknowledgement and credit is given in writing to the effects of lymphatic drainage and the methods used, they have never experienced anything like it previously.
Christine Talbot. SRN. MLD.DLT.
Photographic Healing Diary



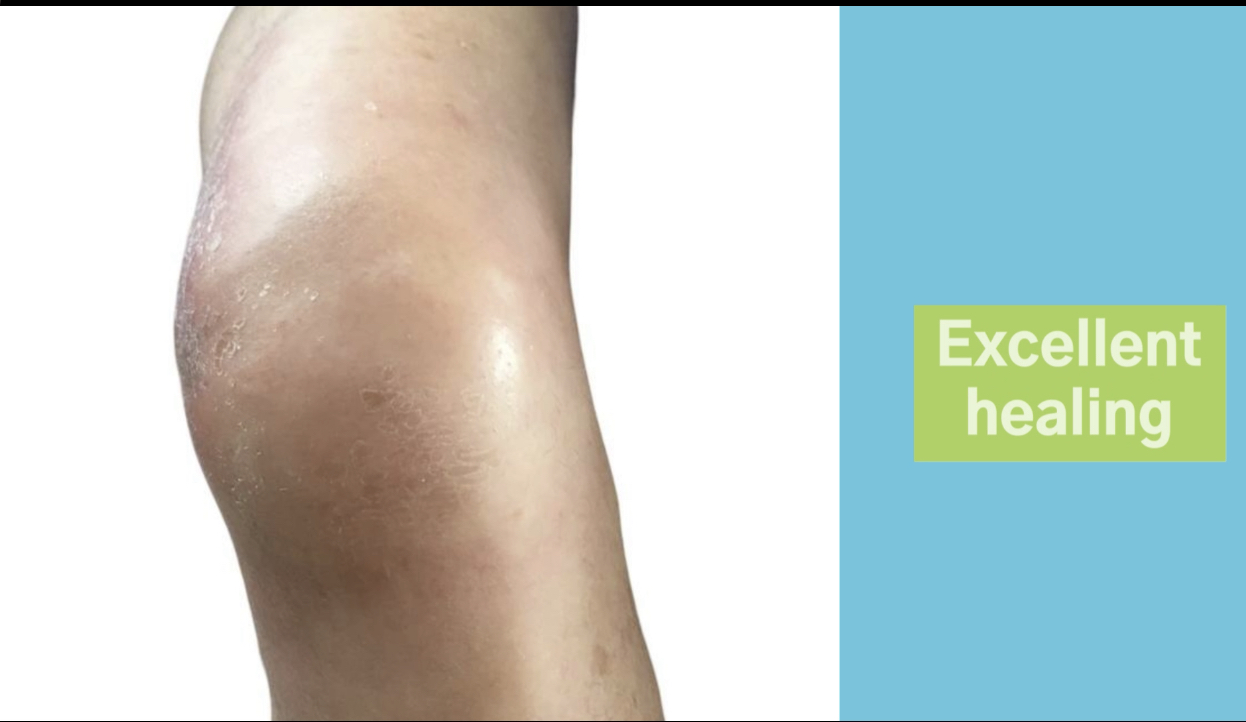


Patient permission received to publish photographs

