Gaynor Leech Guest Blog February 2022
The Journey From Patient to Patient Advocate
"I remember the day of my cancer diagnosis vividly, walking through the corridors of the hospital was like walking through a black narrow tunnel.
I felt claustrophobic and I was scared. My Husband was holding my hand and his voice was very distant, all I could hear from him was “They must have got it wrong.”
Little did I know then, how dramatically my life would change that day. Fortunately, my cancer prognosis was good, I was propelled through my treatment at the speed of light and I will always be grateful to the doctors and nurses who were part of my journey.
.jpg)
Then the unthinkable happened, the very treatment that saved my life produced a side effect called Lymphoedema
I had never heard of Lymphoedema and that it would affect my life in the most unimaginable way. This article is not specifically about Lymphoedema but will give a little insight of the journey from Patient to Patient Advocate. The way I see things, there are three stages that lead to patient advocacy.
The Patient – Stage One
As a patient 11th of May 2011, the day of my Lymphoedema diagnosis, my repeated response of “Lymph What?” and it turned my world upside down. This was something of which I had never heard. It takes a while for a diagnosis of Lymphoedema to sink in, the emphasis was on the 'lifelong and incurable', of management and it appeared that treatment seemed very much secondary.
This was the description of Lymphoedema in my breast cancer folder “Lymphoedema is a long-term complication of some breast surgery, usually when patients have axillary surgery.” My interpretation of this was that surgery alone could cause Lymphoedema and at that time I still did not have a clue.

There was no mention that a side effect of radiotherapy (in my treatment plan),
could cause damage to the lymphatic system leading to development of
Lymphoedema or that there could be any other probable causes.
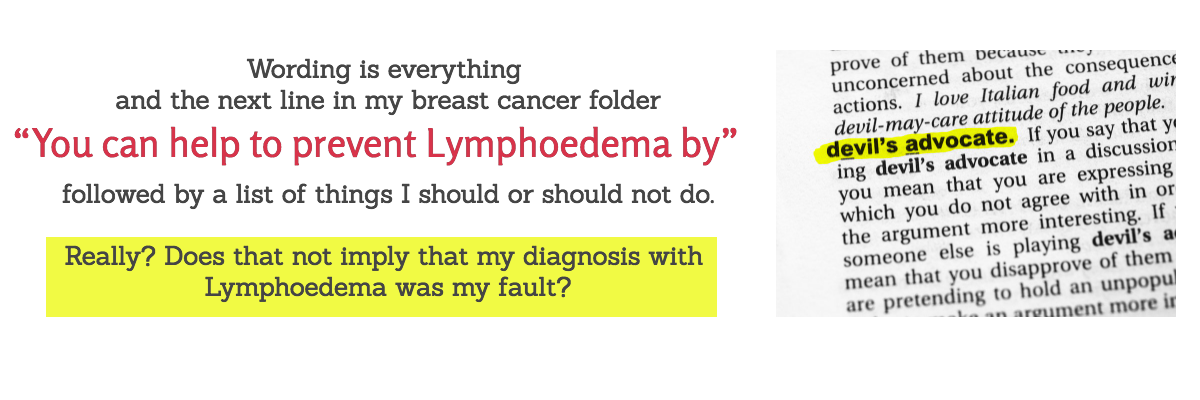
Yes, I am playing Devil’s Advocate here. Anxiety plays a huge part in a Lymphoedema diagnosis and life for patients in the early days are full of ‘what ifs’ and I spent hours wondering what I could have done differently? Remember all this anxiety with Lymphoedema came on the back of a cancer diagnosis. With back-to-back diagnosis of cancer followed by Lymphoedema, logical reasoning did not exist… my head was a mess.
With any health diagnosis as a patient, you will be full of questions, highly likely to be frightened of the impact this will have on your life. Even more frightening is when you ask for advice from your GP or health care provider and they cannot answer your questions. I was lucky that I was able to go to a Lymphoedema clinic and my questions were answered by my specialist nurse, but not all. Then the education began.
Patient Education – Stage Two
The second stage is very much about the patient and how they deal with their diagnosis. My inquisitive mind wanted to understand my diagnosis and so do our members, ‘Dr Google’ scared the living daylights out of me and therefore, I had to look for other answers.
Do look for reputable sources from the Lymphoedema associations in your country and do find a support group to join where you can speak to people in the same position as you. Initially information went over my head, then slowly as I started to get to grips with the research and gain an understanding of what Lymphoedema is, then as Jane Wigg said in her piece, “I was hooked and I became a lymphomanic.”
The diagnosis of Lymphoedema set an unplanned life path. The journey ahead was bumpy. I was not prepared, there was resistance to starting an online support group, not all of its kind and my rebel streak surfaced. I hate it when anyone tells me I should not do something, especially when they cannot give me a logical reason and I do question why. Our members are the same, they want to understand Lymphoedema, they want supported care from our health care providers, they also want to understand how to self care when no supported care is available.
As a patient there is so much to learn about Lymphoedema, but you also need to learn about yourself. How does your Lymphoedema affect you, not just physically but mentally.
These are the questions patients will be asking themselves:
- Which is the right skincare?
- Which is the right compression?
- How do you work a movement plan into a busy day?
- Which lifestyle changes will be effective?
- Where can I find support?
The list of questions is endless and ongoing because one question often leads to another. There is not a one size fits all, we are all different and unique in our own way and patients do remember when you have a terrible day, learn to be kind to yourself.
“You were born to be real, not to be perfect” Ralph Marston
Patient Advocate – Stage 3

The question our group put to Jane Wigg:
Those of us who live with Lymphoedema, wherever that might be in the world are totally frustrated at the lack of understanding in the lymphatic system and lymphatic health. The lack of medical training in this area is appalling, it simply is not part of medical teaching and when it is on the curriculum then there is so little time devoted to the lymphatics. This means as a patient you may not get the answers you are looking for and in the worst-case scenario you may feel that your concerns are not listened to.
Here is one scenario I have personally had to deal with.

On the way to theatre for an operation, a very abrasive anaesthetist told me my information was wrong regarding which arm to use for BP and Cannula. Unfortunately for him, I had checked my facts on the Royal College of Anaesthetist’s the night before and the simple answer was “Not best practice.”
Oops! In recovery after operation, I heard two nurses whispering and all I heard was ‘She’s lovely, no problem.’ They realised I had heard their conversation and came over to apologise for talking about me. They explained because I had challenged the anaesthetist, they assumed I was a troublesome patient.
Misunderstandings, arise easily, our members have numerous stories they can tell. Therefore, I have had to learn to advocate for myself and encourage our members to do the same. In the meantime, we hope all healthcare professionals of the future will learn the amazing job the lymphatic system does and that lymphatic health is the key to our overall health and wellbeing.
Support Groups like L-W-O Community through our website and social media, not only put patients in touch with other patients, but they also encourage chat, questions, and a rant if necessary. The aim is patient empowerment and to give members the confidence to advocate for themselves. Not everyone can do what I do, so for most Lymphoedema patients it is about learning to advocate for themselves.
One of the biggest frustrations from patients is when advice is given, whether that is precautionary or a practical measure, nobody explains why especially when writing fact sheets. When L-W-O provides information on support group, whether that is advice or tips, inevitably someone will ask ‘Why’? Why must I wear compression? Why can’t I go in a hot tub? The list is endless but give patients credit that if you explain the mechanics of why compression works, they are more likely to be compliant. If we simply say you should wear compression because it will reduce your swelling, then do not be surprised if asked ‘Why is that?’
Suggestions that Lymphoedema is not painful because that is what HCP’s may have learnt from their textbooks or the classroom is upsetting. How would anyone know if they do not live with this condition? The line between learning about Lymphoedema and living with Lymphoedema needs to meet in the middle. If your patients question their treatment or ask for more answers, do not be defensive or dismissive, or feel threatened - find a way to come together, embrace the fact that patients will also have an expertise that will also increase your knowledge.
I have seen a huge leap forward with patient associations across Europe and the rest of the world by working together. Lymphoedema patients are helping to drive the fight for recognition. Not only is patient empowerment crucial, but community engagement is also paramount for ourselves and future generations.


xxx

.jpg)
