Understanding Lymphoedema in CRPS
By Victoria Abbott-Fleming, Barrister, Inspirational Speaker & Founder of Burning Nights CRPS Support charity

Complex Regional Pain Syndrome (CRPS) is a debilitating condition and is regarded as a multi-systemic disorder usually involving the limbs that incorporates pain, autonomic, motor, sensory or trophic symptoms which can no longer be explained by the initial trauma.
The condition may develop after trauma, surgery, a minor injury or after a stroke or heart attack.
CRPS is generally categorised into two - CRPS Type 1 and Type 2. There is a third sub-category, CRPS-NOS or CRPS Not Otherwise Specified. Most patients usually fall in Type 1.
Type 1 occurs where there is no direct damage to a nerve, whereas Type 2 occurs when there has been known damage to a nerve. CRPS-NOS occurs in patients who used to fit the diagnostic criteria and now don’t or in patients where their symptoms cannot be better explained.
CRPS is a difficult condition to not only diagnose but to treat. Diagnosis is through a clinical criterion, Budapest Criteria, after all other conditions have been excluded. Doctors will base their diagnosis by looking at a patient’s medical history as well as what they find in a physical examination. X-rays, EMGs and nerve conduction studies may be used when considering a CRPS diagnosis.
Symptoms
Complex Regional Pain Syndrome patients can exhibit a number of symptoms. The leading symptom is CRPS is pain. The pain is usually described by patients as burning, freezing, stabbing and gnawing amongst other descriptions. Other symptoms include:
- Temperature changes
- Colour changes
- Hair, skin or nail changes
- Sweating
- Swelling (oedema)
- Skin sensitivities - hyperalgesia, allodynia, hyperaesthesia etc.
- Decreased range of motion, weakness, tremors, dystonia
CRPS and Oedema
Unfortunately, the pathophysiology of oedema associated with CRPS isn’t fully understood. One of the potential causes of the oedema could be neurogenic inflammation or vasomotor dysregulation.
Other causes of the inflammation and oedema could also be muscle guarding, motor difficulties and immobilisation of the CRPS affected area or limb[1] [2]. CRPS patients often find it difficult to keep their limbs moving because of the pain they feel with movement as well as their general level of pain. Hence the reason why many patients stop using their CRPS affected limb/s. This immobilisation can often lead to further inflammation and oedema.
According to Allen, RJ et al. (2016)[3] the pain, oedema and fibrosis interferes with afferent signalling from the CRPS affected limb, which may then cause further neurological dysfunction and pain sensitization.
Irrespective of where or why the oedema is caused, if the oedematous fluid could be moved away from the affected limb, it may allow for decreased pain and improved range of movement.
Lymphoedema and CRPS
Many people with Complex Regional Pain Syndrome often get misdiagnosed with Lymphoedema instead of CRPS and sometimes vice versa. However, there are some CRPS patients who are diagnosed with Lymphoedema as well as their CRPS.
Lymphoedema is a long-term condition that causes swelling in the body’s tissues, usually caused by a problem in the lymphatic system. We know that CRPS does cause inflammation and oedema in the region where the condition occurs.
If the oedema becomes complex this can lead to Lymphoedema in some patients. Lymphoedema can develop in CRPS patients from the protein-rich fluid that goes to the site of the trauma that may be the initial cause of the CRPS.
The added protein in the fluid can then create a blockage in the lymphatic vessels, which can then prevent it from draining properly. This fluid can then back up behind the blockage which then causes the Lymphoedema and the painful swelling to develop.
The swelling can then lead onto other issues such as skin infections and skin or tissue breakdown.
Managing Oedema CRPS
If a patient has a possible lymphoedema diagnosis, then it may be prudent to consider if they have CRPS instead. Very often it is difficult to distinguish if a patient has oedema from the CRPS or whether it is indeed a complication of the CRPS and it's a separate condition to the CRPS.
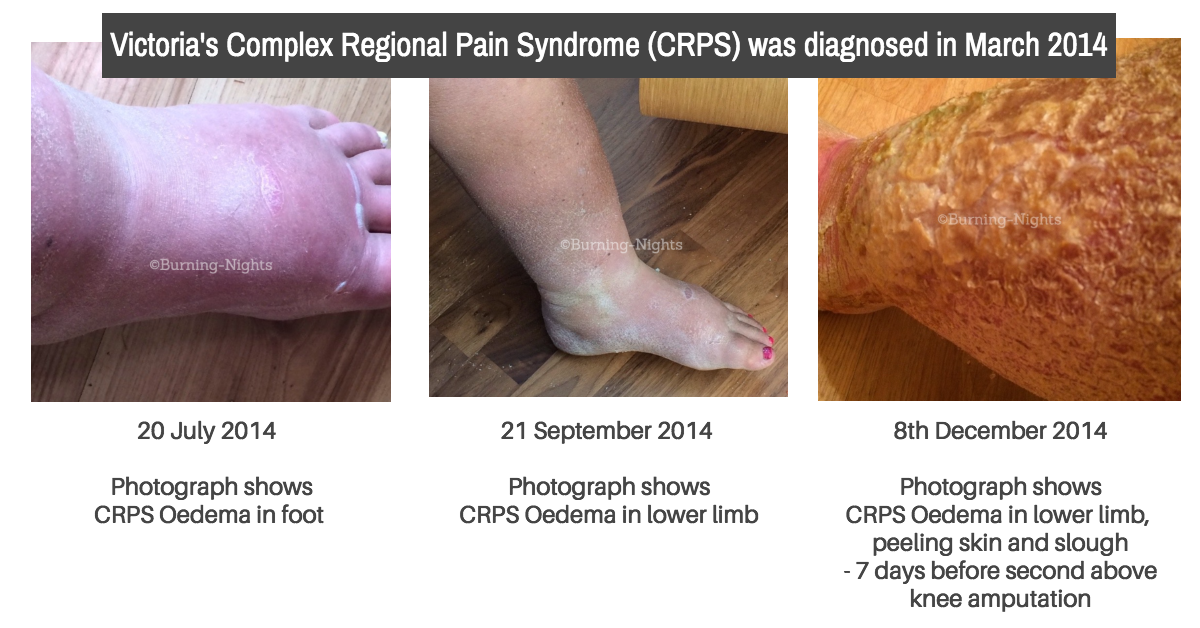
The oedema from CRPS can become very disabling and can impact severely on the quality of life for the patient especially if there is any skin or tissue breakdown or ulceration.
There are only a small number of studies that use Manual Lymphatic Drainage as a treatment for CRPS related oedema such as the 2009 study by Duman I et al[4] which found there was volume reduction immediately after the MLD treatment but it didn’t last over time. In the review study by Allen, RJ et al 2016[5] a small number of MLD studies showed there were conflicting results and they were all isolated treatments instead of part of a comprehensive treatment plan.
Practical Considerations of Lymphoedema Treatments for CRPS Related Oedema
For CRPS related oedema, Lymphoedema treatments may be considered such as compression/Lymphoedema bandaging or Manual Lymphatic Drainage (MLD). However, the patient’s quality of life must be considered and also will the patient be able to cope with the pain from the bandaging or the touching from the MLD.
Many CRPS patients have skin sensitivity symptoms such as hyperalgesia or allodynia, which then may cause issues if compression bandages are being considered. Some patients may not even be able to tolerate having the bandages applied and removed, which could be the same for MLD. Can the patient withstand going through the treatment?
As a charity we have known patients who have had compression bandages to improve their swelling. In one patient, they applied compression bandages over 20 times which after their removal left permanent marks where the bandage overlapped. But it didn't improve their swelling.
Other patients have had compression bandages suggested as a course of treatment but they were not able to withstand the touch of the person applying the bandage nor the touch of the bandage on the skin.[6] In this case the swelling from the CRPS had caused ulcerations which had led to irreversible skin breakdown, and the compression bandaging was not attempted because of the severe allodynia and hyperalgesia. Instead debridement under general anaesthetic was attempted. Unfortunately, the slough from the infection and the open ulcers and tissue returned within 24 hours.
Very often Lymphoedema is misdiagnosed in CRPS patients, when it is simply the CRPS related oedema. Patients are often told to put their limbs up ‘above their heart’ to aid the drainage from the swelling. For CRPS patients, this won’t work and we regularly hear from patients that in fact this doesn’t do anything for the swelling. This leads researchers to believe that it is the vasomotor dysregulation or the neurogenic inflammation that may be the cause of the oedema in CRPS patients.
Conclusion
Understanding how the CRPS affects the person is also important if you are planning on compression bandaging or Manual Lymphatic Drainage. Keeping the patient fully informed at all points is crucial. Allow them to express any concerns they may have about treatment options for the oedema, so questions can be addressed.
As you have read, Complex Regional Pain Syndrome is a very complex condition with a wide range of symptoms including oedema. The CRPS related oedema is often misdiagnosed with Lymphoedema. It is only with using any testing and speaking with the patient that will help with the diagnosis of whether it is Lymphoedema or it is CRPS related oedema.
References
[1] Allen G, Galer BS, Schwartz L. Epidemiology of complex regional pain syndrome: a retrospective chart review of 134 patients. Pain. 1999;80(3):539-544
[2] Harden RN, Oaklander AL, Burton AW, et al. Complex regional pain syndrome: practical diagnostic and treatment guidelines. Pain Medicine. 2013;14(2):180-229.
[3] Allen G, Galer BS, Schwartz L. Epidemiology of complex regional pain syndrome: a retrospective chart review of 134 patients. Pain. 1999;80(3):539-544
[4] Duman I, Ozdemir A, Tan AK, Dincer K. The efficacy of manual lymphatic drainage therapy in the management of limb oedema secondary to reflex sympathetic dystrophy. Rheumatology international. 2009;29(7):759.
[5] Allen, R. J., Armstrong, S. L., Christie, L. F., & Look, J. D. (2016). Lymphedema Therapy for Treatment of Complex Regional Pain Syndrome. risk.
[6] Abbott-Fleming, V. Living with skin complications from complex regional pain syndrome. Wounds UK; 2018,14(5):66-69
Further reading/viewing on CRPS
November 2020 was Complex Regional Pain Syndrome (CRPS) Awareness Month, a poorly understood condition, which affects 1 in 3800 people in the UK and for those affected, the pain is persistent, severe and debilitating. Mary Fickling of PhysioPod contacted Burning Nights, UK Charity and support group after seeing their informative daily graphics on their instagram page to see whether creating a video to keep these facts alive and in the public eye would be helpful?
There is currently no cure for CRPS, but the earlier treatment is received then the better the chances of achieving a remission. Perhaps you recognise these symptoms in yourself or you know someone who is suffering? We wholeheartedly encourage our readers to share this video and to visit the Burning Nights website which holds an array of information and support.
Victoria's Story
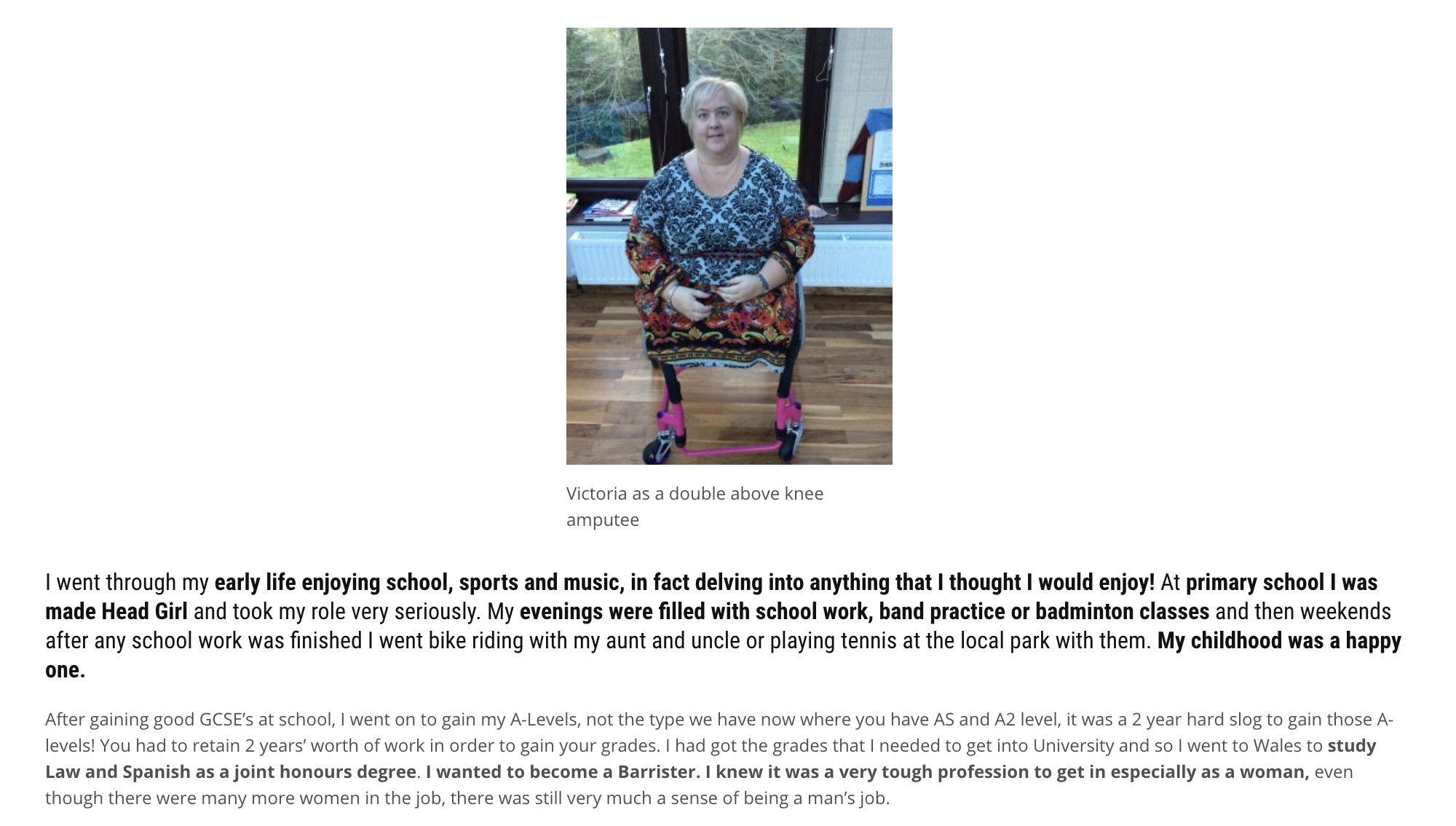
READ VICTORIA'S FULL STORY

