Trauma Related Lymphoedema - A Case Study by Christine Talbot, Lymphoedema and Bowen Practitioner
Previous History:
A fit, very active gentleman in his eighties who regularly plays eighteen rounds of golf and works out daily at a local gym. Mr M owns, self-manages and renovates his properties. Mr M had a number of medical problems over many years for which he had been previously, successfully treated prior to the traumatic injury.
- Cardiac and blood pressure irregularities, cardio vascular disease.
- Mild intermittent claudication.
- Tick bite to his left leg.
- Venous insufficiency on left leg causing discolouration.
- Fall damaging right knee
- Ruptured Baker’s cyst.
- Inflammatory myelitis.
- Choleycystectomy.
- Colitis, investigative colonoscopy with biopsy. A vein was nicked, rushed to hospital, required a blood transfusion of seven units.
- Mild rupture of rectus abdominus.
- Inguinal hernia, considering an operation at some point.
- Mild arterial disease to both legs, well controlled on medication.
I had originally treated Mr M successfully with MLD for an injury and swelling to his right knee.
History:
24th April 2017
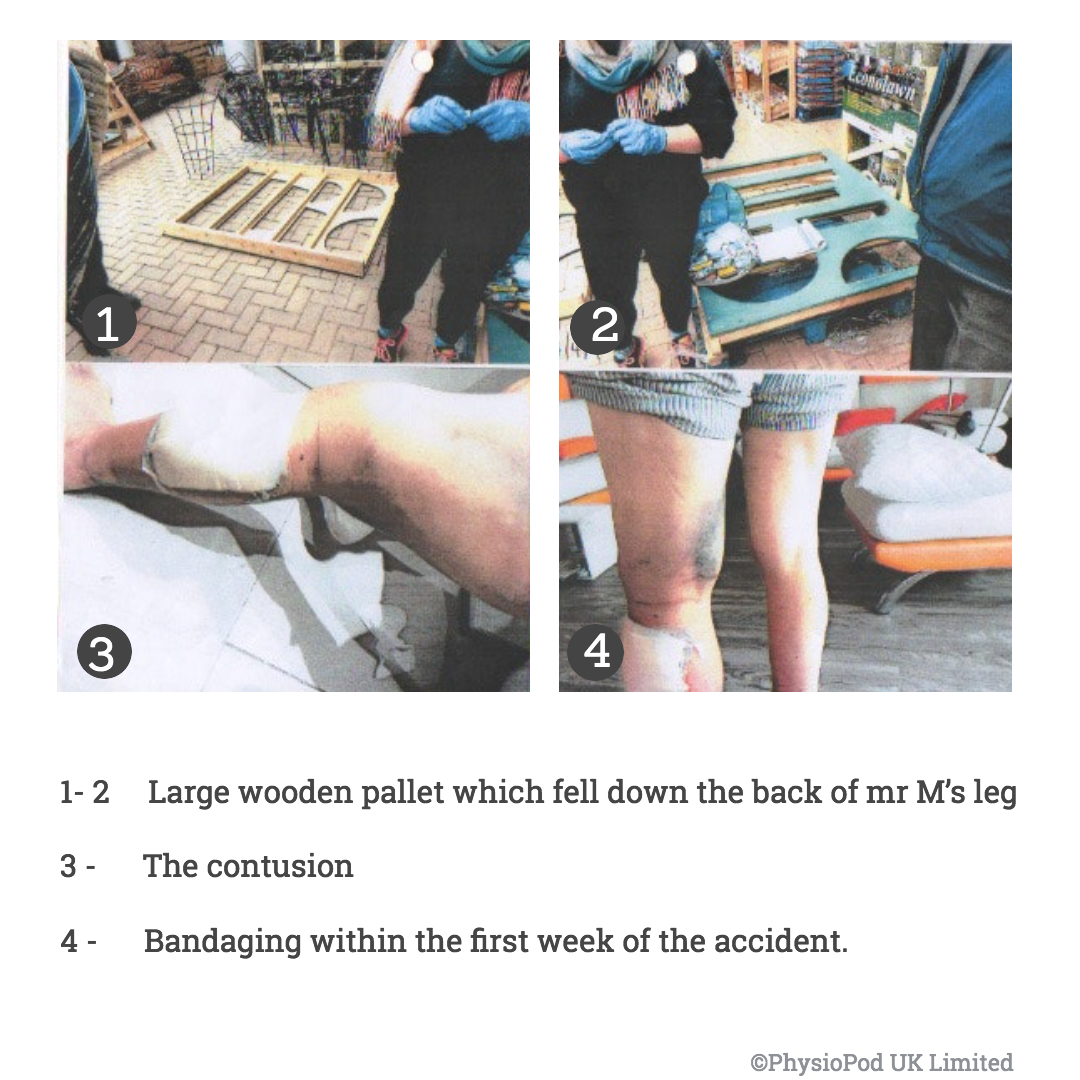
A serious injury occurred to Mr M’s left calf whilst visiting a popular garden centre with his wife and friends. A large wooden pallet which would normally be horizontal at ground level for housing large concrete and terra cotta garden pots was left in a vertical position whilst staff were on a break. A strong gust of wind blew through the area where Mr M was walking and the pallet fell down the back of his left calf. Initially there was no obvious damage or breaking of the skin but in a short time extensive contusion occurred forming a large haematoma with a multiple clot formation. Mr M visited his local hospital in the first week as the wound was leaking blood stained fluid, they applied a bandage. The injury site deteriorated over a short time causing further tissue deterioration and he was prescribed antibiotics, but these were not sufficient and Mr M was admitted to hospital six days after the injury for intravenous antibiotics
Operation 1 -
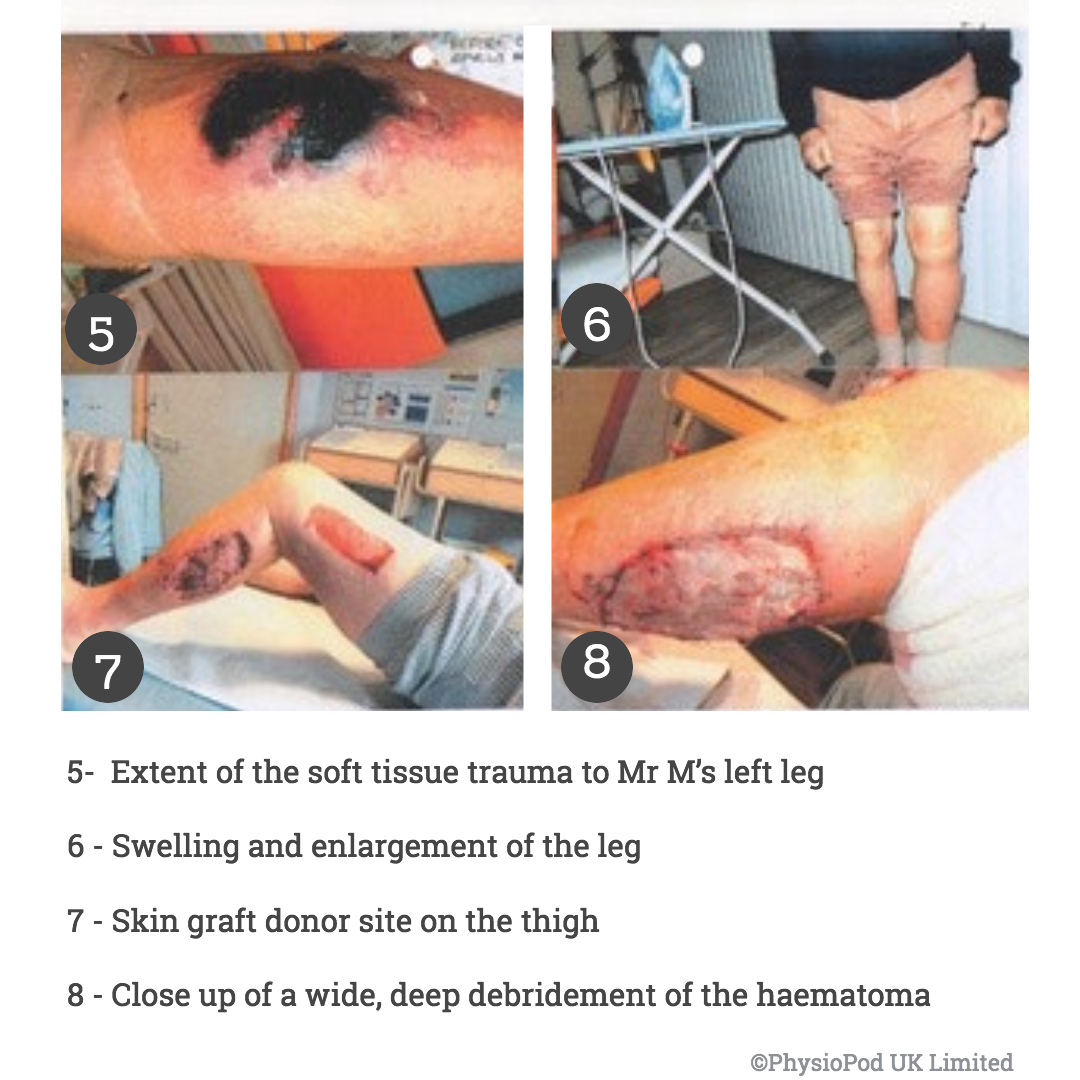
Wide, deep debridement of the haematoma, wound left open with a sponge and pump technique to extract exudate.
Operation 2 -
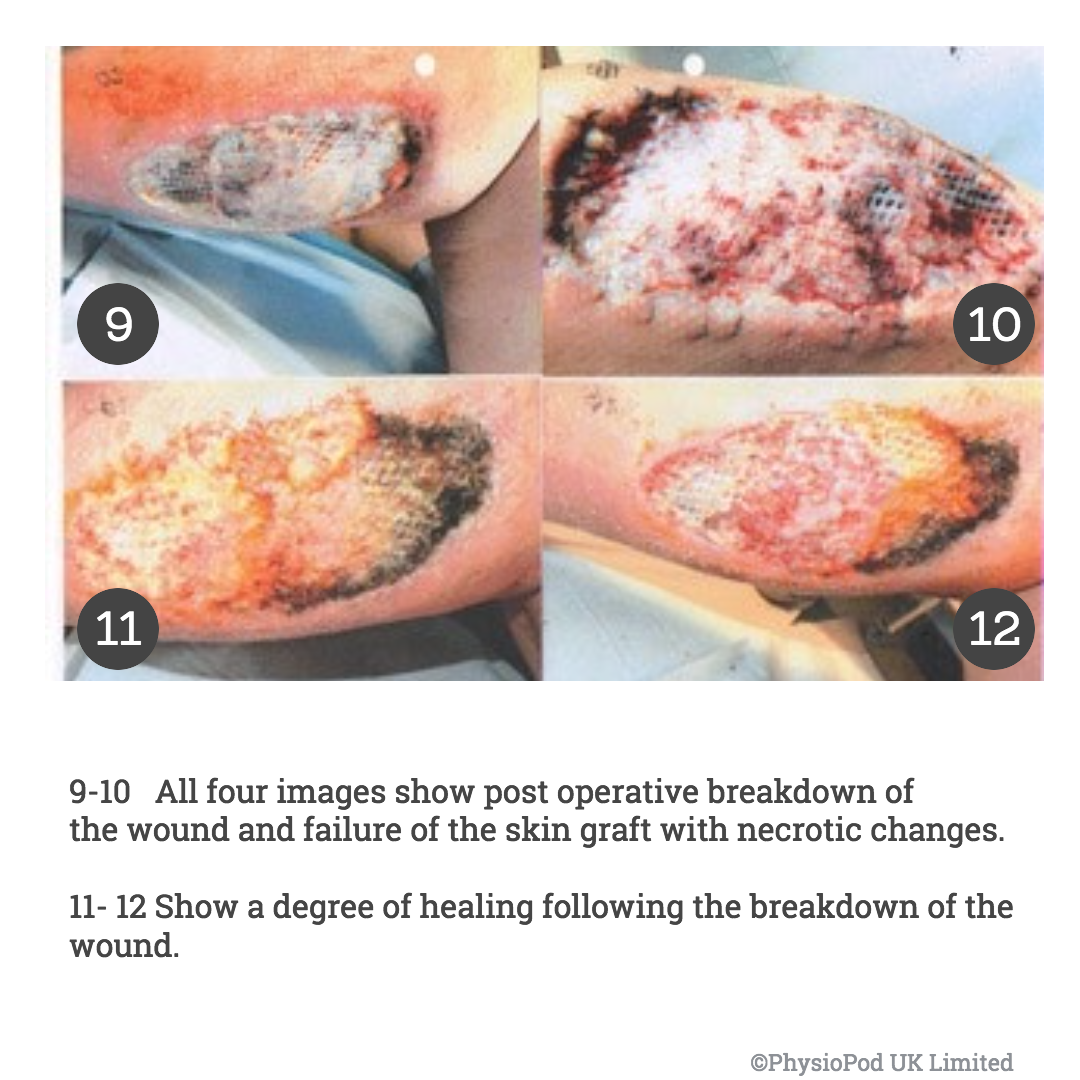
Skin graft taken from left upper lateral thigh, graft clipped to wound site.
Mr M developed cellulitis whilst in hospital and required intravenous antibiotics for several weeks, these have caused pain and intestinal related issues and aggravated his colitis causing abdominal distension made worse due to a weakness in his rectus abdominis muscle.
Manual Lymphatic Drainage: 25th May 2018
Mr M seeks manual lymphatic drainage having remembered how successful the treatment had been for his right knee.
On examination:
A year on from the trauma related incident Mr M has been left with a swollen lower left leg, extensive disfigurement, a dark haemocidrin stain on the site where the cellulitis occurred, loss of muscle mass and limited mobility. There is at the trauma site a deep four to six-inch gauge out of the lateral, posterior calf where the skin graft was applied, the graft infarcted (died) but the decision was to leave it in place and not attempt to re graft as it would be unlikely to take and a second donor site would have to be taken from the right thigh. The graft area is reddened and discoloured and further down the posterior shin is a significant indented area with no discolouration on the lateral aspect of the leg.. There is little movement in the calf, the Achilles is very tight and rigid, the left ankle is thickened and the foot and toes are engorged with fluid.
Treatment:

Quantum Wave Laser to the graft site and calf wound with an excellent response. Magcell to the wound site to encourage blood flow, Deep Tissue Oscillation Therapy 60-152Hz to the neck, abdomen, right leg and affected left leg improving the overall movement even from the first treatment.

On the second appointment Mr M reported a much-improved range of movement at the ankle and was able to walk with greater confidence, the scar area moved more freely over the underlying structure, the donor site was less pronounced but there was still ankle oedema. Treatment was repeated weekly with very encouraging results until July 2018 when Mr M attended a rigorous physiotherapy appointment. The left leg completely regressed, it was very swollen, hardened and reddened and the scar was again indented and took four weeks to resolve made worse by the hot weather and the effects of vasodilation. In the middle of the month Mr M had his first specialist appointment in Exeter with a Dermatologist for an assessment with regards to an insurance compensation claim against the garden centre. It was confirmed the initial lymphatics had been compromised and Mr M thought the specialist was surprised by the extent of the debridement. In August Mr M travelled to see a Plastic Surgeon, in his opinion he considered there would always be a problem with the left leg.
Mr M was further required to travel for other specialist opinions to assess the life changing, limb changing effects upon his life caused by the accident, the consultation fees were hefty for the time given. The fee for a vascular opinion by an Emeritus Professor of vascular surgery for a ninety-minute consultation was approximately £3,299.00, most others were in the region of £1,500-£2,000 for less time. Alas the final award for compensation for a life changing, limb afflicted condition requiring fortnightly self-management funding is not in any way commensurate with these hourly rates, but based on an age-related assumption of minimal need.
Every winter Mr M and his wife leave the UK to holiday in the sun for several months, each time they return there is a deterioration in limb volume which incrementally worsens each year, so too during Covid lockdowns treatment was postponed which was not advantageous to limb management. Mr M is again preparing for his delayed winter break with both legs well maintained plus armed with all essentials to achieve the best outcome in self-management.
Ongoing observations and changes:

Up to a point a good quality of mobility has been maintained with regular assessments, readjustments when required and treating crisis episodes as they occur. Lymph blisters (lymphangiomatas) are apparent on the medial aspect of the lower left leg with a slight cobbling of the skin, as yet there has been no leakage, Mr M has not been able to tolerate hosiery and was not comfortable in an Easy Wrap, he finds a double or triple layer of blue line stockinette most effective as a means of compression. Recently there was a nasty skin break on the mid shin area of the left leg which with Mr M’s vascular history should have rapidly ulcerated, however prior to this I had suggested Mr M take a very good, high quality probiotic as his abdomen was distended and hardened with bowel irregularities and also to use Aveeno skin cream on the cobblestoned dry skin. The speed of healing in a week was remarkable, so I discussed and suggested to other patients of mine with repeated episodes of cellulitis, skin threatening irregularities or areas of limb/skin vulnerability to trial taking probiotics, they have all shown very positive changes in limb and related skin integrity. I first heard about the use of probiotics from an ICU consultant in Oregon who was lecturing on the benefits of lessening and preventing the possibility of sepsis by reinstalling and maintaining a good gut bacteria.

Practitioner conclusion:
It is my opinion, had the initial suggestion to transfer Mr M directly to a Specialist Plastics Unit occurred the outcome would have been less traumatic and less tissue damaging and disabling, instead Mr M was left in limbo waiting on a ward at a local hospital, with his leg festering with no clinical intervention other than antibiotics as by this time he had developed Cellulitis. Mr M’s long-term fitness and manual work ethic has been advantageous in his recovery which makes his ongoing necessity for injury related management more successful. Had Mr M not been so fit and mobile the outcome would most probably have been one of encroaching disability and all that that entails. With continued support and advice from myself Mr M is determined and committed to maintaining his independence at all costs. At the end of the day sadly, this negligent breech in Health & Safety has cost Mr M dearly.
We joke about the SHARK attack to his left leg but this extensive, deep gauge was the work of a SCALPEL, made worse by a probable age-related non-referral to a specialist centre.
Patient Statement:
"The insurance award of £40K was assessed only on the incurred costs and the future needs of medical treatment and did in no way compensate for the great loss of ongoing retirement lifestyle. But from the date of the injury 24th April 2017, I have not been able to return to Golf at all and have had to resign my membership of the IOP Club, also I no longer go to the gym. There was no Health and Safety assessment or report from the Garden Centre and I continue to await the return of my legal costs of over £8,500.
Previously my wife and I were great walkers travelling to places of interest and would enjoy long walks to take in the area’s history, we enjoyed an active social life but my injury and the ongoing complications of that trauma to my leg has brought about an early social change causing a loss of confidence, loneliness for us as a couple and my wife has become a lot more withdrawn. The fate of being in the wrong place at the wrong time is beyond regrettable."
ABOUT DEEP OSCILLATION®
In contrast to externally applied, mechanical forms of therapy, (e.g. vibration), the therapy effect of DEEP OSCILLATION® takes place in the tissue itself and works through the entire depth of the tissue layers (skin, connective tissue, subcutaneous fat, muscles, blood and lymph vessels)
DEEP OSCILLATION® helps in speeding up and improving wound healing processes. Through the oedema-reducing and anti inflammatory effect, the local metabolic elimination and alimentation is improved in all tissue layers, whereby tissue regeneration and wound closure are encouraged on many levels. This is documented by the significant improvement in planimetric and biochemical parameters of the wound healing.
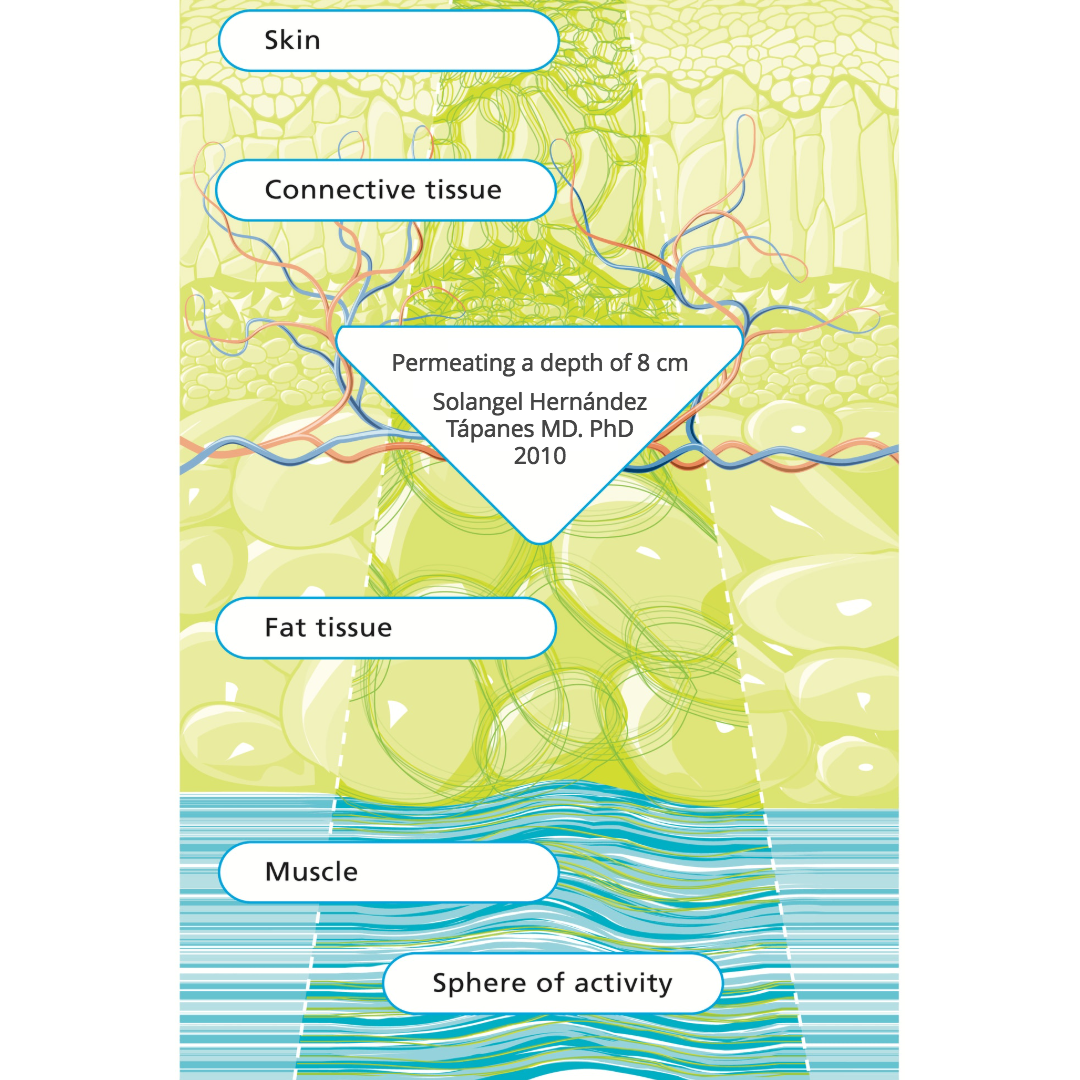
Because of the non-invasive, non-traumatic, gentle nature of this therapy, very early possibilities of application are possible following injury and from Day One post operatively. Chronic conditions can also be worked upon with effective results. Clinical effects [1-26]
About Low level laser therapy (LLLT)
"Low level laser therapy (LLLT) is the use of low energy laser light in injuries and wounds in order to improve wound healing, reduce inflammation and alleviate pain. The laser light is monochromatic, coherent and in the red or near infrared spectrum (600 nm – 1000 nm). It is applied at low power density (1 mW to 500 mW/cm2) (“low energy laser”).
In contrast to other medical laser applications LLLT is not a thermal method (i.e. surgical lasers), but produces photochemical effects in the tissue in a similar way to photosynthesis in plants. LLLT is simple to use, effective and cost-efficient and free of side effects. Treatment takes a few minutes and depending on the indication is repeated at longer or shorter intervals and in accordance with healing success. The success of LLLT is based on the following general action principles: tissue regeneration, inhibition of inflammation, alleviation of pain, improvement in circulation, reduction in swelling" Low-Level-Laser-Therapy (LLLT) in Chronic Wounds - Ludwig-Maximilian University Munich, Germany. Clinical effects [27-31]
About Magcell
Through a patent-registered, innovative procedure, MAGCELL is able to create exceptionally strong pulsating magnetic fields of up to 100 mT (1000 gauss) with selective frequency ranges despite its small size. Time-variable magnetic fields can function as transfer media for electric fields. Providing that – like MAGCELL – the field force is sufficiently high, electro-magnetic fields can be induced in the tissue beyond the internationally recognised threshold for biological effectiveness. Through the possibility of direct application and the resulting close distance of the magnetic field to the application area, MAGCELL® ARTHRO also ensures minimum loss of magnetic field strength, transporting it deep into the tissue layers (electrode-free electrotherapy). Its battery operation and thus constant readiness enables the execution of a therapy programme through repeated short treatments in contrast to treatments previously only offered in doctor’s surgeries.
Magnetic field therapy is available in a range of types and appearances. Various forms of therapy do not have sufficient scientific proof of their effectiveness. The MAGCELL medical product cannot be compared with ‘pulsating signal therapy (PST)’, ‘MultiBioSignal Therapy (MBST)’, Nuclear Magnetic Resonance Therapy’, ‘TENS' or other transmission forms such as magnetic field mats or coils.
MAGCELL works with therapy parameters investigated in empirical and clinical research [32-40]. There are no known side effects or intolerance associated with the use of MAGCELL. Based on a large amount of patient feedback, regular therapy may enable reductions in the dosage of medication, such as non-steroidal anti-rheumatic agents.
Clinical Effects
The following effects of electrode-free electrotherapy with MAGCELL® are clinically recorded:
- Pain alleviation and movement stimulation
e.g. in the case of osteoarthritis - Substantial improvement in circulation
- Reduction of sensory neurotoxicities (polyneuropathy)
- Recently studies showed a very good result by BPH

In blood flow stimulation (Source: Funk et al (2014)
MAGCELL® MICROCIRC significantly increases micro-circulation (p < 0,001) while nitric oxide (NO) has a blood vessel dilatory effect. The authors recommend the therapy for clinical situations where an improvement in micro circulation is identified, like for instance in the case of chronic tissue repair.
References
- Ranzenberger LR, Pai RB. Lymphoscintigraphy. [Updated 2020 Sep 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-.
- Atashkhoei S., Fakhari S. (2016): Management of Breast Cancer Related Lymphoedema. Crescent Journal of Medical and Biological Sciences 3 (4), 111-112.
- Brenke R. - Therapie des Lymphödems EHK 2021; 70: 138-144 DOI - 10.1055/a-1477-817
- Brenke R., Freund R., Strößenreuther RHK (2010): Adjuvant physical therapy for lymphedema and selected comorbidities of the musculoskeletal system. In: Földi M., Földi E. (Ed.): Textbook Lymphology. 7th ed., Elsevier GmbH, 508.
- Brenke R., Siems W. (1996): Adjuvant Therapy for Lymphedema. Lymphol 20, 25-29.
- Flemming D. (2016): The technique of deep oscillation. Lymph self-help, 22-23.
- Gasbarro V., Bartoletti R., Tsolaki E., Sileno S., Agnati M., Coen M., Conti M., Bertaccini C. (2006): Ruolo dell'oscillazione profonda (Hivamat® 200) nel trattamento fisico del linfedema degli arti. La medicina estetica 30 (4), 473-478. English title: The role of deep oscillation therapy (Hivamat® 200) in the physical treatment of the lymphoedema of the limbs.
- GDL (Society of German-speaking Lymphologists) u. DGL (German Society of Lymphology) (2017): AWMF-S2k Guideline "Diagnosis and Treatment of Lymphedema" (AWMF Reg. No. 058-001).
- Jahr S, Schoppe B, Reisshauer A. Effect of treatment with low-intensity and extremely low-frequency electrostatic fields (Deep Oscillation) on breast tissue and pain in patients with secondary breast lymphoedema. J Rehabil Med. 2008 Aug;40(8):645-50. doi: 10.2340/16501977-0225. PMID: 19020698.
- J of IMAB 2016 Jul-Sep;22(3):1248-1252 Improving the quality of life through effects of treatment with low intensity, extremely low frequency electrostatic field with DEEP OSCILLATION® in patients with breast cancer with secondary lymphedema to patients treated with standard lymph equipment. Atanas Petkov1 Corresponding Autor, Yana Kashilska2, Angel Uchikov1, Dean Batzelov3,
- Jui Chu Y. (2017): HIVAMAT 200. In: Jui Chu Y. (Ed.): What Can Physical Therapy Do After Breast Cancer Surgery. CARE, 187-188. German translation: What can physical therapy do after breast cancer surgery.
- Kraus R. (2014): Intensive lymphatic drainage through deep oscillation. LYMPH & Health 2, 6-8.
- Lipiska A., Opuchlik A. (2014): Fizycoterapia w onkologii. In: ?liwi?ski Z., Siero? A. (Ed.): Wielka Fizjoterapia. Elsevier GmbH, 289-294. English title: Physical Therapy in Oncology.
- Mortimer P., Levine G. (2019): Let's Talk Lymphoedema, The Essential Guide to Everything You Need To Know
- Reisshauer A., Pögel S. (2010): Treatment of Secondary Arm Lymphodema in Breast Cancer. Gynecol. prax. 34, 489-499.
- Reißhauer A., Auler S., Bieringer S., year S. (2009): physical decongestive therapy. In: Reißhauer A., Auler S., Bieringer S., year S. (Ed.): Compendium of the lymphological compression supply. Federal School of Orthopedic Technology, 42-57.
- Schingale F.-J. (2006): Head, breast and genital lymphedema - a special challenge for the lymphatic therapist. vasomed 1, 30-31.
- Talbot C. (2011): Lymphoedema Support Network periodical 'Lymphline', Spring Issue, Deep Oscillation for lymphoedema
- Teo I., Coulborn A., Munnock DA (2016): Use of the HIVAMAT® 200 with manual lymphatic drainage in the management of lower limb lymphoedema and lipoedema. Journal of Lymphoedema 11 (1), 49-53
- Theys S., Deltombe T., Legrand C., Hanson P. (2008): Manual Drainage with or without DEEP OSCILLATION® in Lower Extremity Oedema. J Rehabil Med Suppl 47, 62.
- Kraus R. (2014): Intensive lymphatic drainage through deep oscillation. LYMPH & Health 2, 6-8.
- Talbot C. (2011): Lymphoedema Support Network periodical 'Lymphline', Spring Issue, Deep Oscillation for lymphoedema
-
Mosca, R. C., et al. (2019). "Photobiomodulation Therapy for Wound Care: A Potent, Noninvasive, Photoceutical Approach." Adv Skin Wound Care 32(4): 157-167.
-
Machado, R. S., et al. (2017). "Low-level laser therapy in the treatment of pressure ulcers: systematic review." Lasers Med Sci 32(4): 937-944.
-
Tchanque-Fossuo, C. N., et al. (2016). "A systematic review of low-level light therapy for treatment of diabetic foot ulcer." Wound Repair Regen 24(2): 418-426.
-
Kuffler, D. P. (2016). "Photobiomodulation in promoting wound healing: a review." Regen Med 11(1): 107-122.
-
Funk HW, Knels L., Augstein A., Marquetant R., Dertinger HF (2014): Potent Stimulation of Blood Flow of Volunteers after Local Short-Term Treatment with Low-Frequency Magnetic Fields from a Novel Device. Evidence-Based Complementary and Alternative Medicine 2014. Article ID 543564, 9 pages. http://dx.doi.org/10.1155/2014/543564 .
-
Geiger G., Mikus E., Dertinger H., Rick O. (2015): Low frequency magnetic field therapy in patients with cytostatic-induced polyneuropathy: A phase II pilot study. Bioelectromagnetics 36 (3): 251-254. doi: 10.1002 / bem.21897.
-
Hitrov NA, Portnov VV (2008): MAGCELL® ARTHRO in the treatment of osteoarthritis in the knee joint. Naturopathy 3, 25-27.
-
Leoci R., Aiudi G., Silvestre F., Lissner E., Lacalandra GM (2014): Effect of Pulsed Electromagnetic Field Therapy on Prostate Volume and Vascularity in the Traetment of Benign Prostatic Hyperplasia: A Pilot Study in a Canine Model. The Prostate 74: 1132-1141.
-
Reimschüssel A., Bodenburg P. (2009): Low-frequency electromagnetic fields. Successful in the therapy of myoarthritis of the temporomandibular joint. Naturopathy 5, 28.
-
Rick O., von Hehn U., Mikus E., Dertinger H., Geiger G. (2017): Magnetic Field Therapy in Patients With Cytostatics-Induced Polyneuropathy: A Prospective Randomized Placebo-Controlled Phase-III Study. Bioelectromagnetics 38 (2): 85-94 :. doi: 10.1002 / bem.22005.
-
Wuschech H., von Hehn U., Mikus E., Funk RH (2015): Effects of PEMF on patients with osteoarthritis: Results of a prospective, placebo-controlled, double-blind study. Bioelectromagnetics 36 (8), 576-585.

