The Efficacy and Safety of Deep Oscillation in the Management of Post-Mastectomy Pain Syndrome: A Case Series
Presented by Lic. Rosario Pineda at the XXI World Congress of the International Union of Phlebology (UIP) in Buenos Aires in 2025. A prestigious event for professionals in the fields of phlebology and lymphology.
The author Lic. Rosario Pineda declared that she has no conflict of interest in this presentation and is sharing professional experience for educational purposes and not for commercial gain. The work was carried out by the Rosario Leg Institute from 2015 to 2025 in Argentina.
Author: Lic. Rosario Pineda Affiliations: International Agency for Research on Cancer (WHO)
Introduction and Background
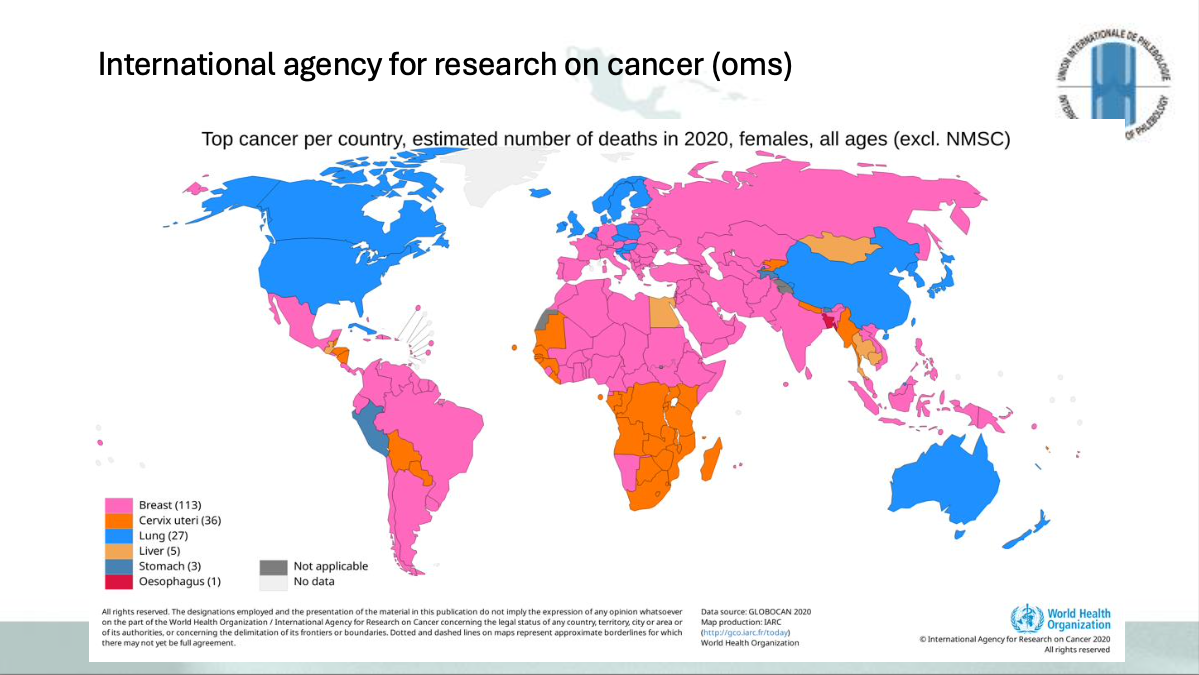
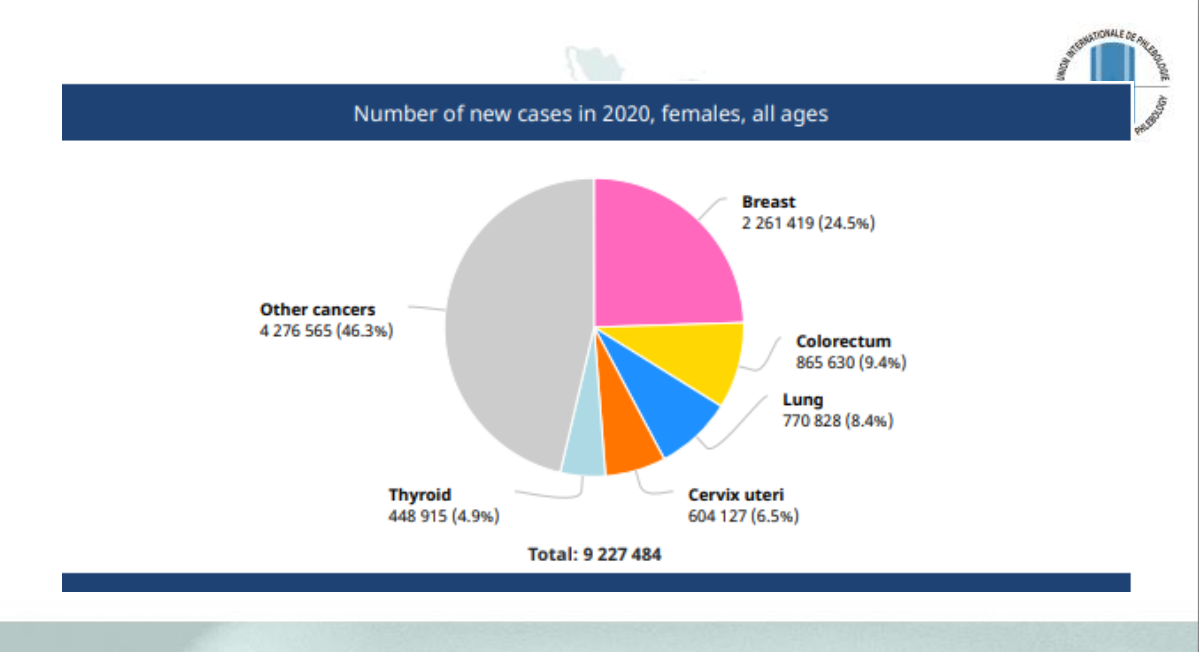
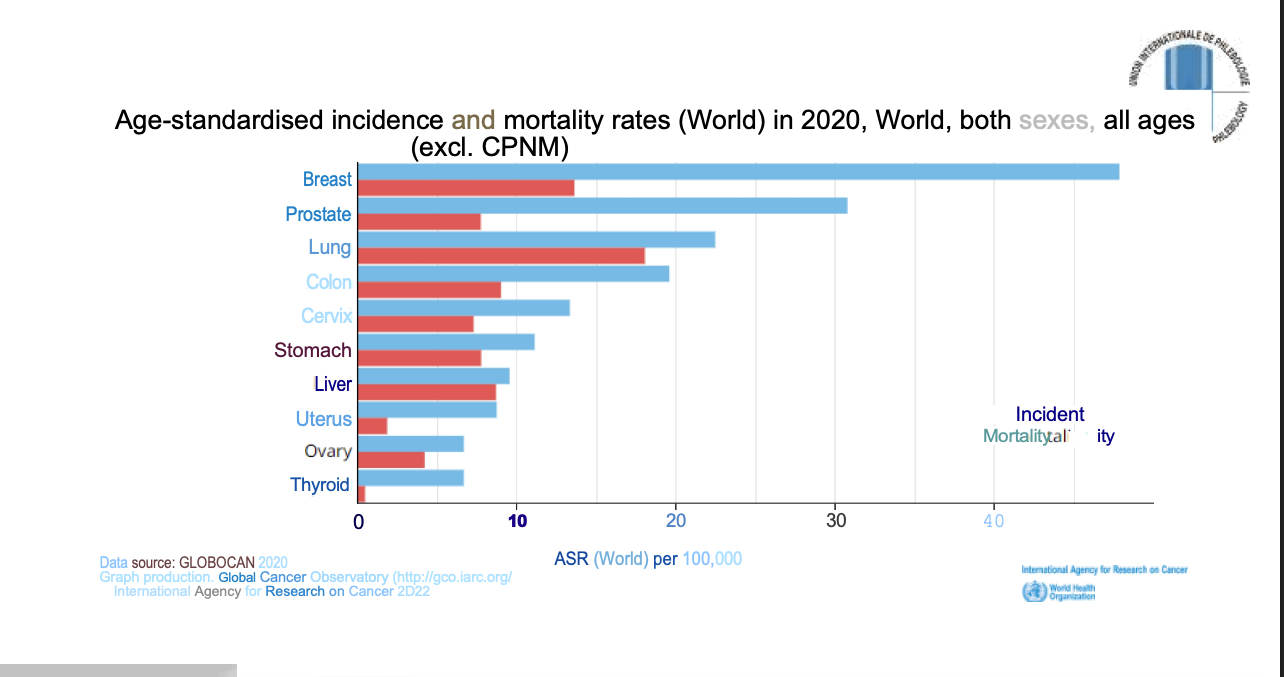

Globally in 2020, breast cancer was a significant health concern, contributing to a total of 9,227,486 cases across various cancers (excluding CPNM, based on age-standardised incidence and mortality rates). Medical treatment for breast cancer typically involves surgery, radiotherapy, and chemotherapy.
A common complication following surgical intervention is Post-Mastectomy Pain Syndrome (PMPS).
The International Association for the Study of Pain (IASP) defines PMPS as persistent pain that appears after a breast surgery. This pain affects the front of the chest, the ipsilateral breast upper arm, and the armpit. It may be exacerbated by movements of the shoulder girdle. The pain intensity is often described as moderate to severe and is characteristically neuropathic pain.
PMPS can persist for months or even years following a mastectomy. Prevalence rates vary significantly across publications, ranging from 4% to 100%, with other reports citing ranges of 11–57%. Importantly, 65% of patients present with neuropathic characteristics. PMPS is likely secondary to injury to the intercostobrachial or intercostal nerve during lymph node dissection at the axillary level, and it may or may not be accompanied by Axillary Network Syndrome.
Study Design and Methodology
This presentation is based on an OBSERVATIONAL STUDY conducted over 10 years, from JANUARY 2015 to MARCH 2025, structured as a CASE SERIES. Informed consent was obtained from all participating patients. The work was carried out by the Rosario Leg Institute.
The objective of the work was to reduce PMPS pain and restore the patient to their Activities of Daily Living (ADLs).
Patient Cohort and Criteria
The study included N=33 patients (32 women, 1 man), with an average age ranging from 35 to 60 years.
- Inclusion criteria: Patients who had undergone breast cancer surgery or reconstructive breast surgery after breast cancer, and who presented with SDPM, with or without axillary network syndrome.
- Exclusion criteria: Seromas, fibromyalgia, spinal disc herniation, rheumatoid arthritis, and shoulder pathologies.
Assessment Tools
Assessment utilized validated scales and physical evaluations:
- Informed consent and Anamnesis.
- Pain assessment: Validated scales, including the Lattinen Index (which measures pain, frequency, analgesic use, night-time sleep, and inability to perform ADLs).
- Session-specific evaluation: The Visual Analogue Scale (VAS).
- Functionality assessment: The Upper Limb Functional Scale.
- Physical evaluation: Goniometry, inspection, and palpation.
Kinesiological Treatment Objectives
The overarching goals of the kinesiological treatment were to mitigate PSMS pain, thereby improving the quality of life, and to stimulate and improve limb movement and functionality. Furthermore, treatment aimed to improve healing and return the patient to their ADLs.
Deep Oscillation: Mode of Action and Application
Deep Oscillation (DO) was utilized as the core intervention. This equipment generates a low-intensity, non-thermal intermittent electrostatic field (U=100-400V, I 150 µA) with a very low frequency (5–250 Hz rectangular biphasic).
The mechanism involves the electrostatic field attracting the patient's tissue at the selected frequency and then separating it, creating a pumping effect in the treated area through rhythmic deformations (Mratskova, 2020; Petkov, Kashilska, Uchikov, C Batzelov, 2016). Unlike conventional electrotherapy, which acts on the neuromuscular system, deep oscillations act primarily on connective tissue, with effects measured up to 8 cm deep by ultrasound.
Safety and Therapeutic Effects
The sources highlight the safety and specific effects of Deep Oscillation in the context of cancer patients:
- Safety: Due to its very low frequencies, DO is not capable of stimulating cellular activity, including metastatic cells, thus ensuring safety for cancer patients (Petkov, Kashilska, Uchikov, C Batzelov, 2016).
- Microcirculation and Lymphatics: DO acts on microcirculation, enhancing blood flow in the interstitial space (Teo, Coulborn, Munnoch, 2016; Boisnic C Branchet, 2013). The electrostatic field causes channels to open, releasing free radicals and metabolic by-products accumulated in the extracellular space, which are then captured by the lymphatic system (Jahr et al. 2008).
- Pain Reduction: The mode of action in pain reduction related to peripheral nerve damage includes the Gate control theory (Christian, Koenig, Winkelmann, C Games, 2019). It offers rapid and long-lasting pain relief (Mratskova, 2020). It also decreases the expression of TRPV1 receptors present in sensory neurons, which are often increased following inflammatory processes (Boisnic C Branchet, 2013). Pain relief is also achieved through the removal of algogenic substances (like prostaglandins and ROL) via lymphatic pumping (Koleva, Ioshinov, C Yoshinov, 2017).
Treatment Protocol Employed
The kinesiological treatment utilized only Deep Oscillation Pro equipment (high and low frequencies), which is NON-IONISING. Treatment involved 2 weekly sessions during the first month, 1 session per week during the second month, and 1 session every 15 days thereafter, if necessary. Stretching exercises and skin desensitisation treatments for neuropathic pain were recommended as daily home support. The application technique required the use of vinyl gloves.
Example Application Schedule (Times and frequencies used may vary depending on tissue condition):
|
Period |
Frequencies Used |
Total Time |
|
Week 1 (3 sessions, every other day) |
5 min at 160 Hz, 5 min at 80–120 Hz, 2 min at 160 Hz |
12 minutes of application |
|
Week 2 (up to first month, 2 sessions per week) |
8 min at 160–180 Hz, 5 min at 80–120 Hz, 2 min at 160 Hz, 5 min at 15–40 Hz |
20 minutes of application |
Results
Significant improvements were observed in the cohort of 33 patients.
Pain Improvement: Pain improvement was noted using the VAS scale by the 10th session.
Results at 3 Months:
- Pain reduction was maintained, with VAS scores decreasing drastically (from 9 to 1).
- There was complete improvement in shoulder and arm functionality.
- Muscular strength was regained.
- Patients successfully returned to their daily activities and physical activities in gyms and/or sports.
Conclusion
The findings from this case series indicate that an early specialised approach and treatment is highly effective in reducing pain in patients with PMPS.
Deep, very low-frequency oscillations are an effective and safe adjuvant therapy for the treatment of SDPM.
The results underscore the undisputed importance of vascular rehabilitation within the transdisciplinary team to enhance the evolution and recovery after breast cancer surgery, ultimately improving the quality of survival and ensuring a rapid return to daily activities.
Scientific References
- Post-Mastectomy Pain Syndrome (PMPS) and Cancer Epidemiology
- Chatterjee A, Pyfer B, Czerniecki B, Rosenkranz K, Tchou J, Fisher C. Early postoperative outcomes: lumpectomy versus simple mastectomy. J Surg Res 2015;198(1):143–8. DOI: 10.1016/j.jss.2015.01 mastectomy. J Surg Res 2015;198(1):143-8. DOI: 10.1016/j.jss.2015.01.054.
- Couceiro TC, Valenca MM, Raposo MC, Orange FA, Amorim MM. Prevalence of postmastectomy pain syndrome and associated risk factors: A cross-sectional cohort study. Pain Manag Nurs 2014;15(4):731-7, DOI: 10.1016/ j.pmn.2013.07.011.
- Di Sibio, A., Abriata, G., Forman, D., & Sierra, M. S. (2016). Female breast cancer in Central and South America. Cancer Epidemiology, 44, S110-S120.
- Ferlay J, Soerjomataram F Ervik M, Dikshit R, Eser S, Mathers C, et al. GLOBOCAN 2012v1.1, Cancer incidence and mortality worldwide: IARC Cancer Base No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer; 2014. Available at: http://globocan.iarc.fr [accessed on 5 October 2016].
- International Association for the Study of Pain (IASP). Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. The International Association for the Study of Pain, Subcommittee on Taxonomy. Pain 1986;3:S1-226.
- Ramirez-Parada, K., Mella-Abarca, W., Nicoletti-Santoni, N., Torres-Riveros, G., Villagran-Gutierrez, I., Petric-Guajardo, M., & Aguilera-Eguia, R. (2019). Implementation of an early and prospective kinesiological care model in people with breast cancer. Journal of Surgery
- Reuben SS, Makari-Judson G, Lurie SD. Evaluation of efficacy of the perioperative administration of venlafaxine XR in the prevention of postmastectomy pain syndrome. J Pain Symptom Manage 2004;27(2):133-9.
- Vilholm OJ, Cold S, Rasmussen L, Sindrup SH. The postmastectomy pain syndrome: an epidemiological study on the prevalence of chronic pain after surgery for breast cancer. Br J Cancer 2008;99(4):604–10. DOI: 10.1038/sj.bjc.6604534.
- Waltho D, Rockwell G. Post-breast surgery pain syndrome: Establishing a consensus for the definition of post-mastectomy pain syndrome to provide a standardised clinical and research approach - a review of the literature and discussion. Can J Surg 2016;59(5):342-50.
- Deep Oscillation and Related Therapies
- Boisnic S, Branchet MC. Anti-inflammatory and draining effect of the Deep Oscillation® device tested clinically and on a model of human skin maintained in survival condition. Eur J Dermatol. 2013 Jan-Feb;23(1):59-63. doi: 10.1684/ejd.2012.1904. PMID: 23420030.
- Christian, McCall E.; Koenig, Riley C.; Winkelmann, Zachary K.; and Games, Kenneth E. (2019) "The Effects of Deep Oscillation Therapy for Individuals with Lower-Leg Pain," Journal of Sports Medicine and Allied Health Sciences: Official Journal of the Ohio Athletic Trainers Association: Vol. 4: Iss. 3, Article 3. DOI: https://doi.org/10.25035/jsmahs.04.03.0
- DeLeon, P. H. (2016). A Systematic Review of Deep Oscillation and a Study Proposal of its Effects on Geriatric Bedridden Patients with Lower Extremity Lymphedema.
- Jahr S, Schoppe B, Reisshauer A. Effect of treatment with low-intensity and extremely low-frequency electrostatic fields (Deep Oscillation) on breast tissue and pain in patients with secondary breast lymphoedema. J Rehabil Med. 2008 Aug;40(8):645-50. doi: 10.2340/16501977-0225. PMID: 19020698.
- Kashilska Y., Petkov A., P. Micheva, Batashki A., Batashk Z. (2015): Improving the quality of life through effects of treatment with low-intensity extremely low-frequency electrostatic field with DEEP OSCILLATION® in patients breast cancer with secondary limb to patients treated with standard lymphatic equipment. Medicine V(1), 381-387.
- Koleva, I. B., Ioshinov, B. R., & Yoshinov, R. D. (2017). Complex Analgesia (Infiltrations and Deep Oscillation) in Patients with Stump Pain and Phantom Pain after Lower Limb Amputation (Double-blind Randomised Controlled Trial of Efficacy). Journal of Advances in Medicine and Medical Research, 22(11), 1-17. https://doi.org/10.9734/JAMMR/2017/34198
- Mratskova, Galina. (2020). USE OF DEEP OSCILLATION -THERAPY IN REHABILITATION PROGRAM FOR PATIENT AFTER DISTAL RADIUS FRACTURE WITH A COMPLEX REGIONAL PAIN SYNDROME: A CASE REPORT. Trakia Journal of Sciences. 18. 187-193. 10.15547/tjs.2020.s.01.034.
- Pogorzelska, J. A., Zaglaniczny, D., Zmyslna, A., & Kiebzak, W. (2017). Observation of deep oscillation usage and its effectiveness on burn scars—case report. Medical Studies/Studia Medyczne, 33(1), 46–50.
- Teo, I., Coulborn, A., & Munnoch, D. A. (2016). Use of the HIVAMAT 200® with manual lymphatic drainage in the management of lower-limb lymphoedema and lipoedema. Journal of Lymphoedema(11), 49-53.
- Z. K., Roberts, E. J., & Games, K. E. (2018). Acute Effects and Perceptions of Deep Oscillation Therapy for Improving Hamstring Flexibility. Journal of sport rehabilitation, 27(6), 570-576.
Contact Details: Licrosariopineda@gmail.com
Instagram: Maríadelrosario.pineda

