Alamoudi, U., Taylor, B., MacKay, C., et al. (2018). Submental liposuction for the management of lymphedema following head and neck cancer treatment: a randomized controlled trial. Journal of Otolaryngology - Head & Neck Surgery, 47(1), 22. https://doi.org/10.1186/s40463-018-0263-1
Arends, C.R. et al. (2024). Lymphedema and Trismus After Head and Neck Cancer, and the Impact on Body Image and Quality of Life. Cancers, 16(3), p.653. DOI: https://doi.org/10.3390/cancers16030653
Atar, S. et al. (2023). The efficacy of Kinesio Taping on lymphedema following head and neck cancer therapy: A randomized, double blind, sham-controlled trial. Physiotherapy Theory and Practice, 39(9), pp.1832–1846. DOI: https://doi.org/10.1080/09593985.2022.2056862
Borges, M.M.F. et al. (2023). Photobiomodulation therapy in the treatment of radiotherapy-related trismus of the head and neck. Lasers in Medical Science, 38(1), p.259. DOI: https://doi.org/10.1007/s10103-023-03920-0
Chalasani, R. & McNab, A. (2010). Chronic Lymphedema of the Eyelid: Case Series. Orbit, 29(4), 222–226. https://doi.org/10.3109/01676831003695735
Cheng, J.T. et al. (2023). Rehabilitation interventions for head and neck cancer-associated lymphedema: a systematic review. JAMA Otolaryngology–Head & Neck Surgery. DOI: https://doi.org/10.1001/jamaoto.2023.1473
Deng, J. et al. (2021). Photobiomodulation Therapy in Head and Neck Cancer-Related Lymphedema: A Pilot Feasibility Study. Integrative Cancer Therapies, 20. DOI: https://doi.org/10.1177/15347354211037938
Halliday, E., Gittins, J. & Ahsan, S.F. (2020). Using the Glasgow Benefit Inventory questionnaire to quantify the health benefits of lymphoedema treatment in patients with head and neck cancer. Applied Cancer Research, 40(9). DOI: https://doi.org/10.1186/s41241-020-00093-y
Jeans, C. et al. (2023). A prospective, longitudinal and exploratory study of head and neck lymphoedema and dysphagia following chemoradiotherapy for head and neck cancer. Dysphagia, 38(4), 1059–1071. DOI: https://doi.org/10.1007/s00455-022-10526-1
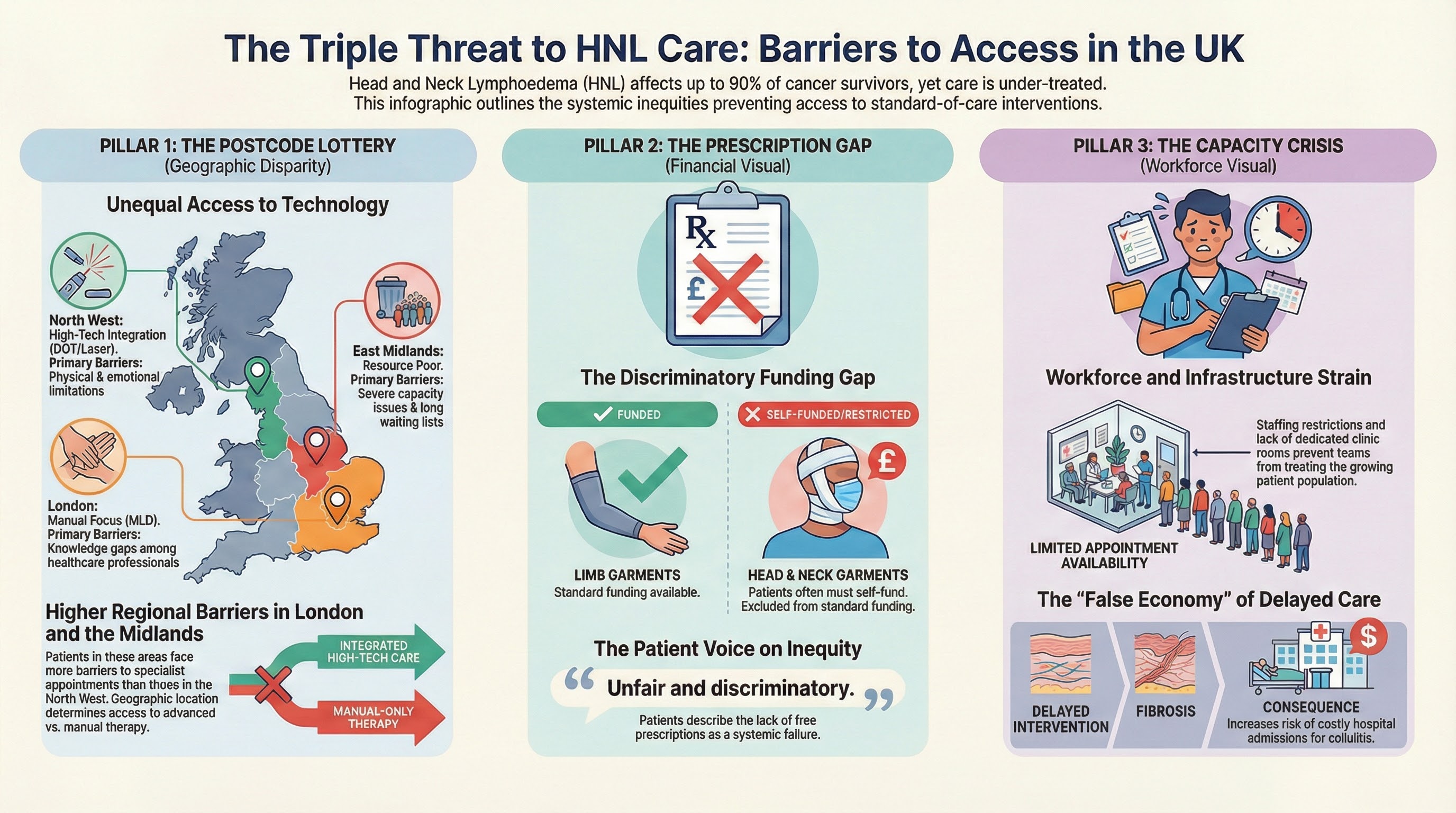
Julka-Anderson, N. et al. (2026). Late effects services for adults living with and beyond cancer: a scoping exercise of the current provision in the UK. Cancer Nursing Practice, 25(1). DOI: https://doi.org/10.7748/cnp.2026.e1904
Mayrovitz, H. N., Ryan, S., & Hartman, J. M. (2018). Usability of advanced pneumatic compression to treat cancer-related head and neck lymphedema: A feasibility study. Head & Neck, 40(1), 137–143. https://doi.org/10.1002/hed.24995
Mihara, M., Uchida, G., Hara, H. et al. (2011). Lymphaticovenous anastomosis for facial lymphoedema after multiple courses of therapy for head-and-neck cancer. Journal of Plastic, Reconstructive & Aesthetic Surgery, 64(9), 1221–1225. https://doi.org/10.1016/j.bjps.2011.01.006
Mullan, L.J. et al. (2025). Evaluating the effects of lymphoedema management strategies on functional status and health-related quality of life following treatment for head and neck cancer: a systematic review. Journal of Cancer Survivorship, 19(1), 121–139. DOI: https://doi.org/10.1007/s11764-023-01453-7
Rajaram, R. et al. (2025). The Management of Head and Neck Lymphoedema: A 2025 Systematic Review. Head & Neck, 47(10), 2897–2910. DOI: https://doi.org/10.1002/hed.28265
Ridner, S., Dietrich, M. S., Niermann, K., Cmelak, A., Mannion, K., & Murphy, B. (2016). A prospective study of the lymphedema and fibrosis continuum in patients with head and neck cancer. Lymphatic Research and Biology, 14(4), 198–205. https://doi.org/10.1089/lrb.2016.0001
Ridner, S.H. et al. (2021). Advanced pneumatic compression for treatment of lymphedema of the head and neck: a randomized wait-list controlled trial. Supportive Care in Cancer, 29, 795–803. DOI: https://doi.org/10.1007/s00520-020-05540-8
Shah, N. (2025). 'As a maxillofacial surgeon, I never expected to get mouth cancer myself'. British Dental Association, News and Opinion. Available at: https://www.bda.org/news-and-opinion/blog/as-a-maxillofacial-surgeon-i-never-expected-to-get-mouth-cancer-myself
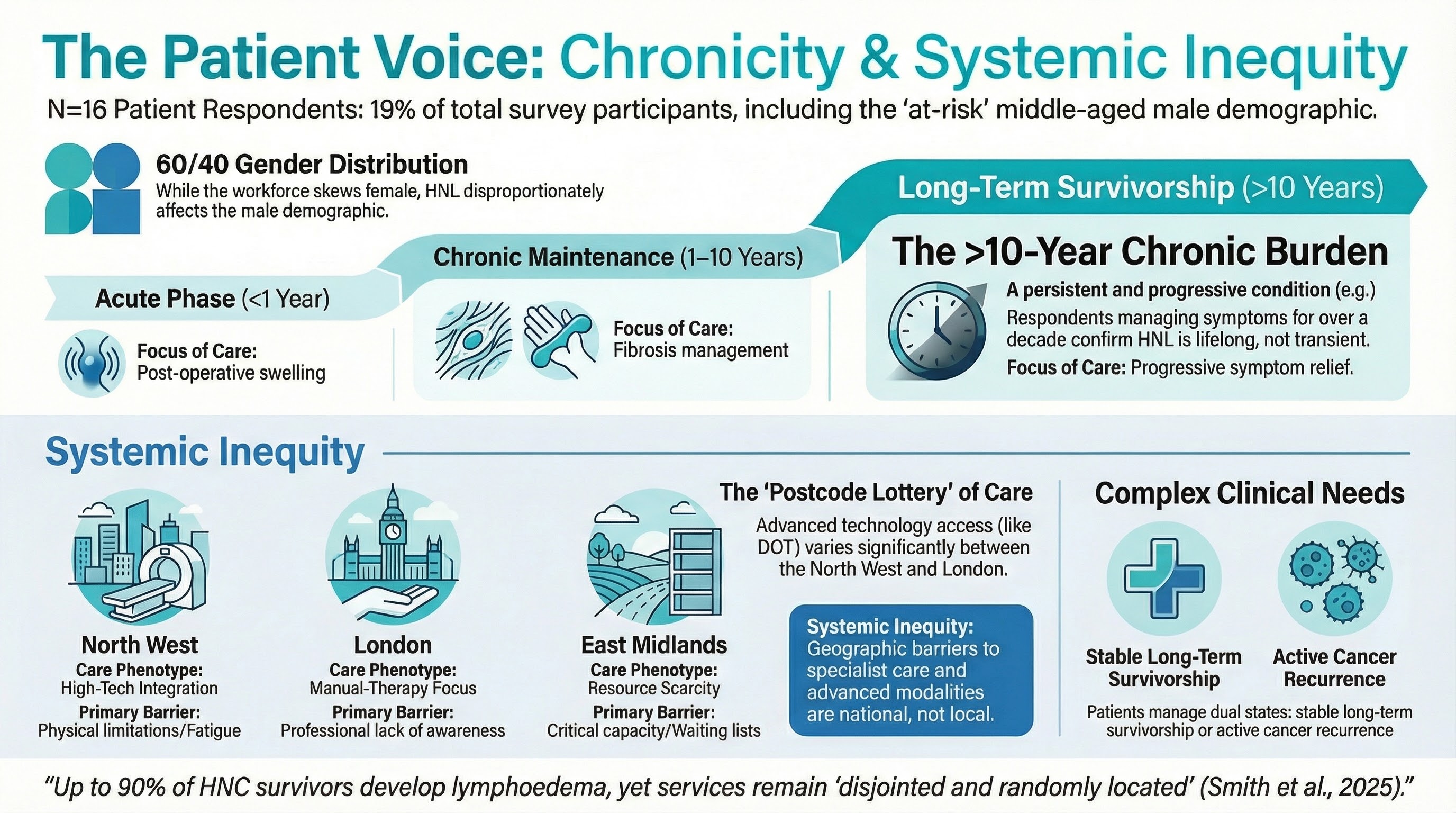
Smith, A.J., Cherry, M.G. & Patterson, J. (2025). Head and neck lymphoedema service provision in the UK: a survey of practice. Supportive Care in Cancer, 33(12), 1142. DOI: https://doi.org/10.1007/s00520-025-10107-6
Starmer, H.M. et al. (2023). Head and neck lymphedema and quality of life: the patient perspective. Supportive Care in Cancer, 31(12), 696. DOI: https://doi.org/10.1007/s00520-023-08150-2
Suami, H. et al. (2019). A new indocyanine green fluorescence lymphography protocol for identification of the lymphatic drainage pathway for patients with breast cancer-related lymphoedema. BMC Cancer, 19, 985. DOI: https://doi.org/10.1186/s12885-019-6192-1
Tsai, K.Y. et al. (2022). Effect of early interventions with manual lymphatic drainage and rehabilitation exercise on morbidity and lymphedema in patients with oral cavity cancer. Medicine (Baltimore), 101(42):e30910. DOI: https://doi.org/10.1097/MD.0000000000030910
Tyker, A. et al. (2019). Treatment for Lymphedema Following Head and Neck Cancer Therapy: A Systematic Review. American Journal of Otolaryngology, 40(5), 761–769. DOI: https://doi.org/10.1016/j.amjoto.2019.05.024
Venchiarutti, R.L. et al. (2023). Treatment approaches and outcomes of a head and neck lymphedema service at an Australian comprehensive cancer center. Head & Neck, 45(6), 1539–1548. DOI: https://doi.org/10.1002/hed.27369
Warren, A.G. & Slavin, S.A. (2007). Scar Lymphedema: Fact or Fiction? Annals of Plastic Surgery, 59(1), 41–45. DOI: Annals of Plastic Surgery
Wigg, J. & Cooper, G. (2017). How is lymph fluoroscopy mapping altering lymphoedema management? British Journal of Community Nursing, 22(Sup10), S16–S20. DOI: https://doi.org/10.12968/bjcn.2017.22.Sup10.S16
Wood, K., Hopper, S., Murray, M. C., Alston, J., Paul, O., Jefferson, G. D., Jackson, L. L., & Kane, A. C. (2025). Feasibility and efficacy of home-based lymphedema exercises for head and neck cancer patients at a safety net hospital. American Journal of Otolaryngology, 46(1), 104560. https://doi.org/10.1016/j.amjoto.2024.104560
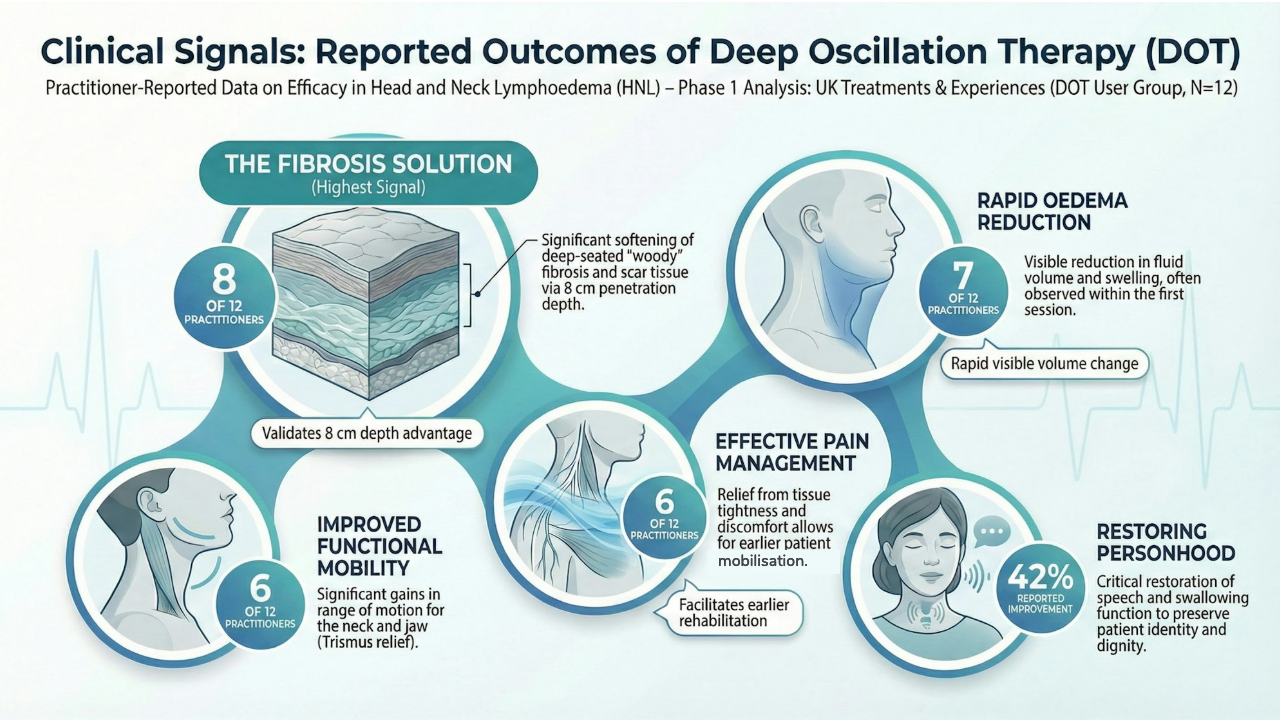
Deep Oscillation Therapy (DOT) Specific References
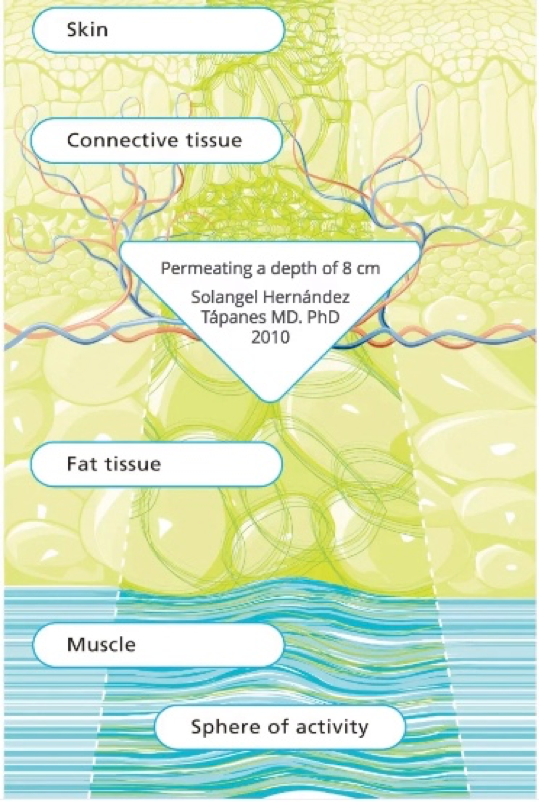
Hernández Tápanes, S. et al. (2018). The Effect of Deep Oscillation Therapy in Fibrocystic Breast Disease: A Randomized Controlled Clinical Trial. International Archives of Medicine, 11(14). DOI: https://doi.org/10.3823/2555
Hernández Tápanes, S. et al. (2010). Value of deep oscillation therapy in the healing of AB burns. Cuban Journal of Physical Medicine & Rehabilitation, 2(1). URL: DO Solangel 2010 Burns
Reinhold, J. (2025). Deep Oscillation. In: Cornely M. E. et al. (eds.), Applied Lymphology. Springer Nature Switzerland AG. DOI: https://doi.org/10.1007/978-3-031-77734-9_40
Economic, Wound Care & Service Provision References
Guest, J.F., Fuller, G.W. & Vowden, P. (2020). Cohort study evaluating the burden of wounds to the UK’s National Health Service in 2017/2018. BMJ Open, 10(12). DOI: https://doi.org/10.1136/bmjopen-2020-045253
Lian, Y. & Atkin, L. (2025). Addressing the lack of compression therapy provision in NHS Hospitals across the UK. Wounds UK, 21(1). URL: https://wounds-uk.com/journal-articles/addressing-the-lack-of-compression-therapy-provision-in-nhs-hospitals-across-the-uk/
Webb, E. et al. (2023). Compression Therapy Is Cost-Saving in the Prevention of Lower Limb Recurrent Cellulitis in Patients with Chronic Edema. Lymphatic Research and Biology, 21(2), 160–168. DOI: https://doi.org/10.1089/lrb.2022.0029
Key Guidelines (Available Online)
British Lymphology Society (BLS). (2024). Manual Lymphatic Drainage Position Document. Available at: https://www.thebls.com/documents-library
Health Service Executive (HSE) & Lymphoedema Network Northern Ireland (LNNI). (2022). All-Ireland Lymphoedema Guidelines for the Diagnosis, Assessment and Management of Lymphoedema. [Online]. Available at: https://www.hse.ie/lymphoedema OR https://lnni.org/
Sustainability Directory. (2025). Brain’s Waste Fluid Drains through Newly Discovered Lymphatic Vessels in the Nose (Nasopharyngeal Lymphatic Plexus). Referencing Findings in Nature (2025). https://news.sustainability-directory.com/research/brains-waste-fluid-drains-through-newly-discovered-lymphatic-vessels-in-the-nose/