'Invisible Disabilities' By Nichola Ebbern, Head of Health and Safety at Shepherds Bush Housing Association

I am disabled and you wouldn’t know it if you met me.
I am not alone. In Great Britain in 2012, there were 5.7million disabled people of working age (figure 1) and while there are no formal figures on those with disabilities that are not visually recognisable, research suggests this is as high as 80%. Coincidentally, I became disabled in 2012, which means I became one of the approximately 4.5 million people living with an invisible disability.
I look like the average person but I definitely don’t feel like it!
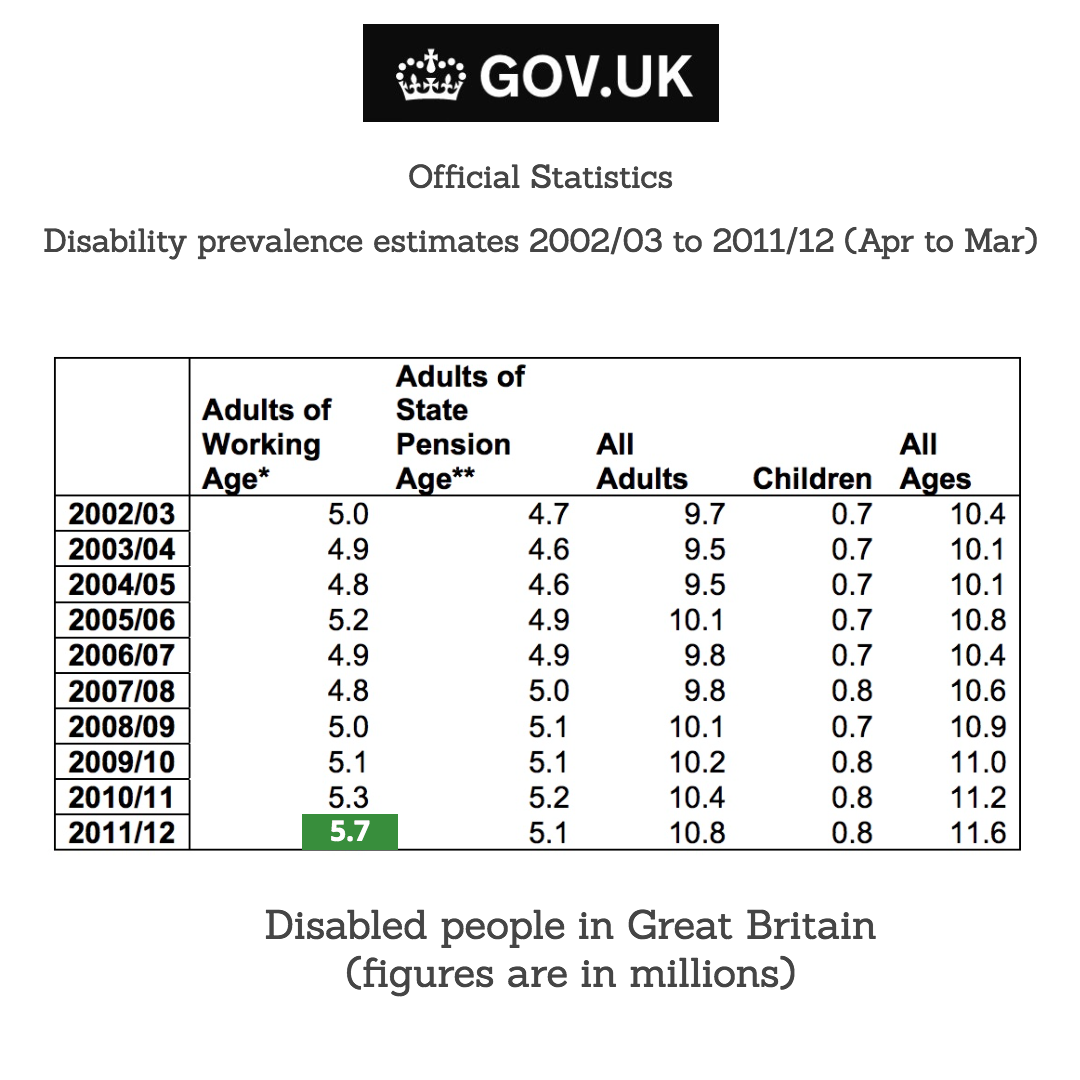

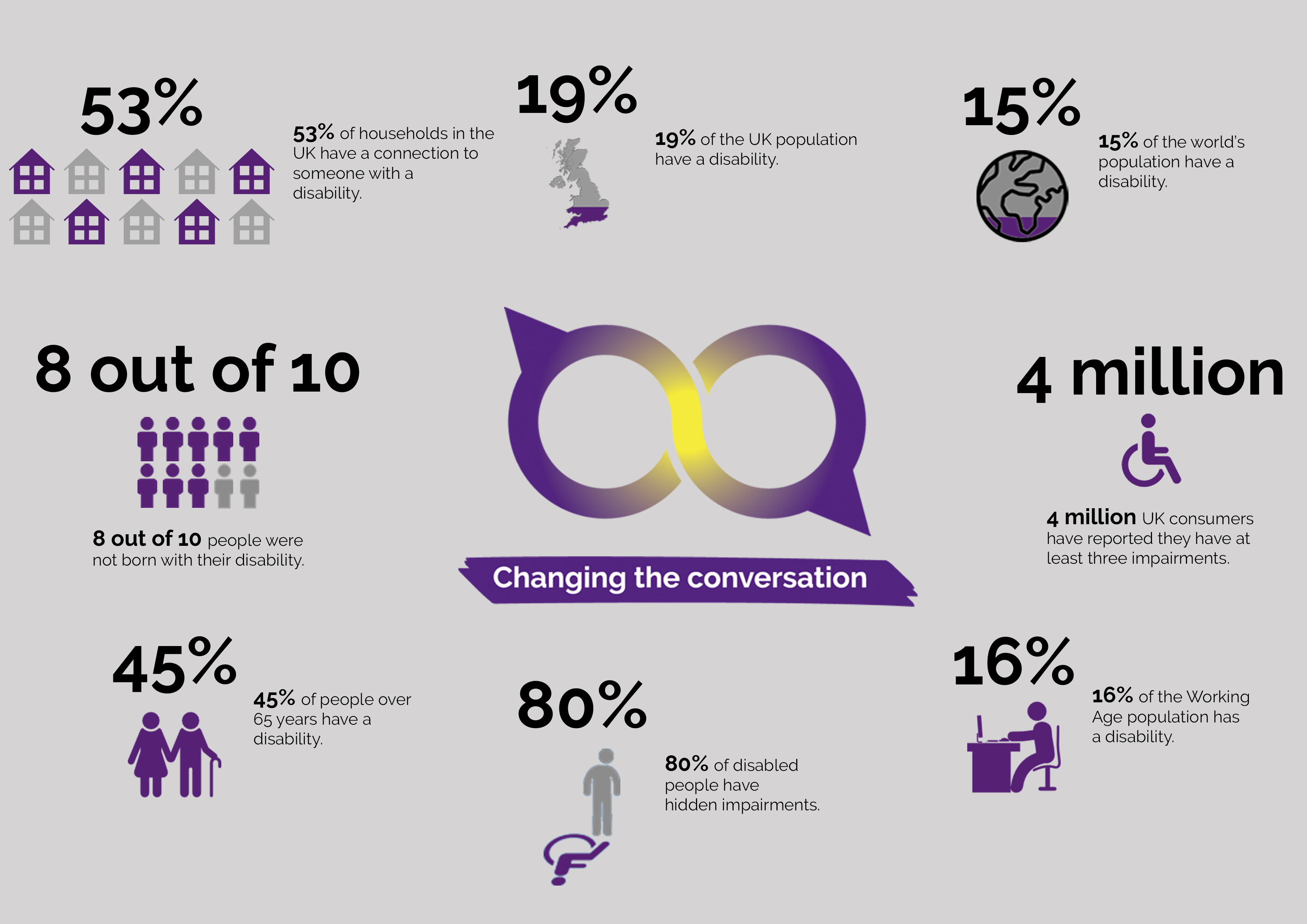
Figure 2: Facts and Figures from Purple Pound - 80% of disabled people have hidden impairments (August 2020)
COVID-19 Lockdown & Reassessment of Priorities
Like many people, I have hidden my disability in the workplace because of the stigma, but one of the benefits of the COVID-19 lockdown has been time for reflection and reassessment of priorities. I feel that I’ve moved forward significantly on my personal journey and I’ve come to realise that I’ve got a useful story to tell. I want to help others to address the unspoken topic of invisible disabilities and making work 'a more equal and fairer' place to be.
In 2012, I was diagnosed with breast cancer – I was unusually young: according to the Government, in 2015 there were 1.8 million people living with a cancer diagnosis and only 7.6% of these were under 44. Like many women and men with breast cancer, following on from my operations I had chemotherapy and radiotherapy followed by years of taking tablets.
Cancer-related fatigue (CRF) is a prolonged, distressing and subjective sense of physical, emotional or cognitive exhaustion associated with cancer or its treatment [3]. Studies of long-term cancer survivors suggest that approximately one-quarter to one-third experience persistent fatigue for up to 10 years after cancer diagnosis [4,5]. Chronic fatigue is linked to so many illnesses, some of which result in a formal disability and others are chronic conditions, such as chronic fatigue syndrome (CFS/ME), complex regional pain syndrome (CRPS) or chronic pain, fibromyalgia, congestive heart failure, diabetes, chronic obstructive pulmonary disease (COPD) etc and of course now we have long-COVID. There are many people in the workplace managing their energy budgets on a day-to-day basis.
Cancer-related fatigue (CRF) cannot be sorted with a good nights sleep
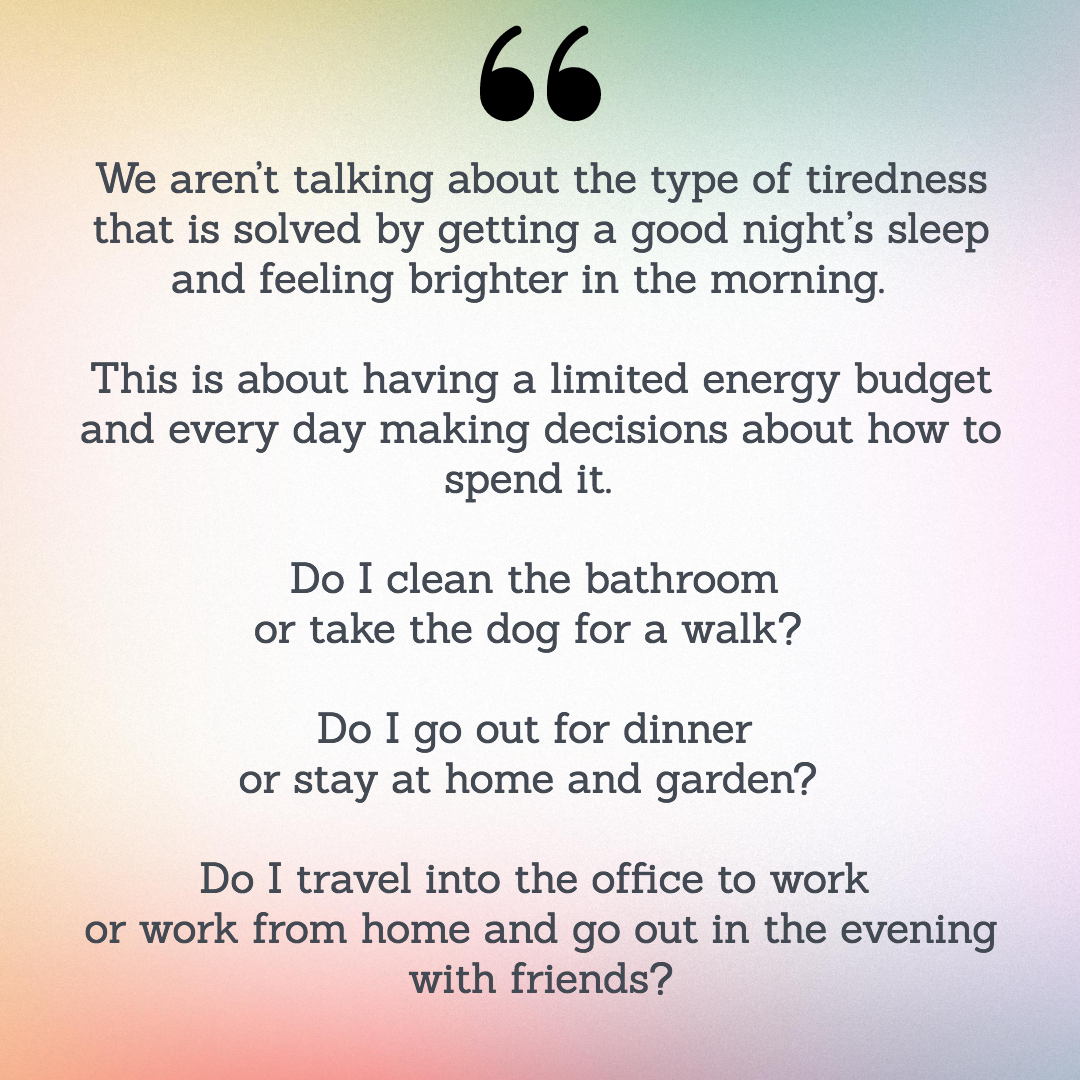
As you can imagine, this has a massive impact on all aspects of my life. I have come to realise how interconnected my physical and mental health are and how I’m on a sliding scale of wellness every day. Small things in one part of my life can have a massive impact on other areas.

"An unfortunate connection - unfortunately, people who have chronic fatigue may become depressed. And while depression doesn’t cause chronic fatigue syndrome, it can certainly cause increased fatigue" [6]
Other research links increased physical activity (within an individual’s limits) with improved mental health and energy levels. "There are many reasons why physical activity is good for your body – having a healthy heart and improving your joints and bones are just two, but did you know that physical activity is also beneficial for your mental health and wellbeing? [7]
I’ve found both of these things to be true and this is where my other long-term health condition comes to the fore (Figure 3). Secondary Lymphoedema is a swelling of the arm (or other body area) and in my case, it is caused by removal of the lymph nodes in my armpit during cancer surgery.
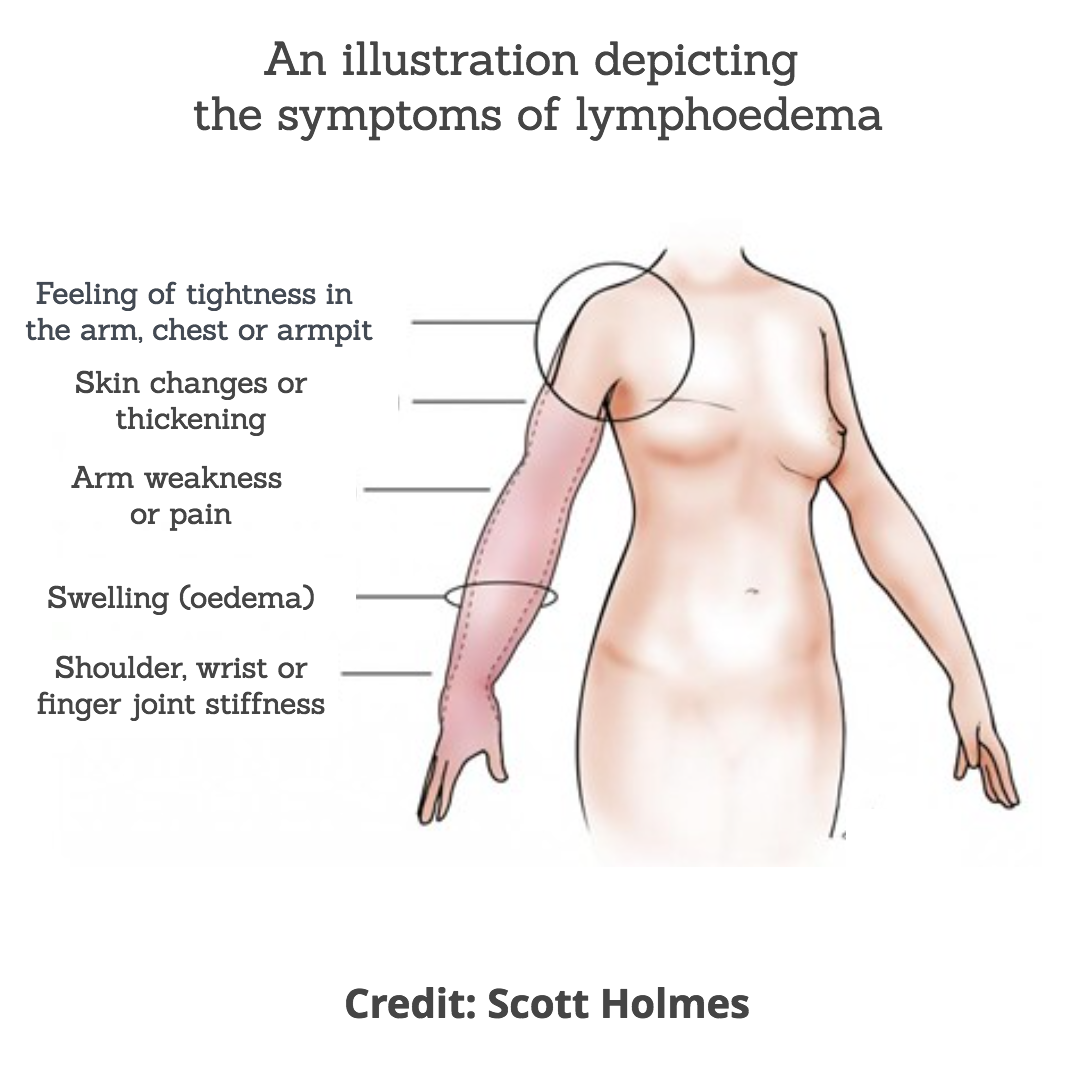
Figure 3 - Secondary Lymphoedema Symptoms following treatment for breast cancer
According to reports the incidence of breast cancer related lymphoedema (BCRL) varies and is approximately 20% at one year and increases to 40% at ten years after breast cancer treatment, with a cumulative incidence of 28% [8,9]
There is no cure for Lymphoedema, and for most, management of the condition is through compression garments and Manual Lymphatic Drainage (MLD) which is only available privately.
The cancer related fatigue means that I don't run anymore; running use to be a major stress management tool and I ran on average about 30/40 miles a week every week, until 2012. I now need to balance what, and how much activity I undertake, with the increased pain and suffering I experience.
Luckily I was referred to Christine Talbot some years ago for private MLD by an acquaintance and I can honestly say this was a turning point in my lymphoedema treatment. Christine encouraged me to continue with physical activity and especially classes like Les Mills BODYPUMP™ in order to build muscle strength and improve lymphatic drainage. This advice was diametrically opposed to the original advice I was given by the NHS – 'don’t exercise, limit the use of your arm, avoid lifting weight'.
Thankfully, I understand this is not now the advice given and that exercise is now a key part of lymphoedema care and maintenance [10].
DEEP OSCILLATION® as a self care tool for Lymphoedema
Christine also introduced me to Deep Oscillation Therapy (Figure 4) and see study references [11-34] - she uses this electrostatic field therapy in her treatments. I live quite a way from Christine but I was fortunate enough to be able to purchase my own machine. I still see Christine but having the machine at home means I am able to manage my condition much more proactively. Having the support of an excellent MLD practitioner and my own machine has meant I’m able to be much more active, which in turn supports my fatigue.

Figure 4: Deep Oscillation treatment is now supplied in to many NHS Lymphoedema Services
ASKING FOR UNDERSTANDING
If you have an invisible disability, help your line manager to help you by being open and honest so that they can understand you, see the challenges in your life and work with you to help you achieve your peak performance both at home and at work. It’s scary but it's worth it!

References
- Disability prevalence estimates 2011/12
- 1 in 5 of the UK population are disabled and 80% of these people have a hidden disability - Purple Pound, August 2020
- Bower JE. Cancer-related fatigue--mechanisms, risk factors, and treatments. Nat Rev Clin Oncol. 2014;11(10):597-609. doi:10.1038/nrclinonc.2014.127
- Bower JE, et al. Fatigue in long-term breast carcinoma survivors: a longitudinal investigation. Cancer. 2006;106:751–758.
- Servaes P, Gielissen MF, Verhagen S, Bleijenberg G. The course of severe fatigue in disease-free breast cancer patients: a longitudinal study. Psychooncology. 2007 Sep;16(9):787-95. doi: 10.1002/pon.1120. PMID: 17086555.
- Fatigue and Depression: Are They Connected? Healthline 2021
- Paluska, S.A. & Schwnek, T.L. (2000). Physical Activity and Mental Health: Current Concepts. Sports Med, 29 (3), 167–180.
- Rebegea L, Firescu D, Dumitru M, Anghel R. The incidence and risk factors for occurrence of arm lymphedema after treatment of breast cancer. Chirurgia (Bucur). 2015 Jan-Feb;110(1):33-7. PMID: 25800313
- DiSipio T, Rye S, Newman B, Hayes S. Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol. 2013 May;14(6):500-15. doi: 10.1016/S1470-2045(13)70076-7. Epub 2013 Mar 27. PMID: 23540561.
- Marchica P, D'Arpa S, Magno S, Rossi C, Forcina L, Capizzi V, Oieni S, Amato C, Piazza D, Gebbia V. Integrated Treatment of Breast Cancer-related Lymphedema: A Descriptive Review of the State of the Art. Anticancer Res. 2021 Jul;41(7):3233-3246. doi: 10.21873/anticanres.15109. Epub 2021 Jul 5. PMID: 34230117.
- Atashkhoei S., Fakhari S. (2016): Management of Breast Cancer Related Lymphoedema. Crescent Journal of Medical and Biological Sciences 3 (4), 111-112.
- Brenke R. - Therapie des Lymphödems EHK 2021; 70: 138-144 DOI - 10.1055/a-1477-817
- Brenke R., Freund R., Strößenreuther RHK (2010): Adjuvant physical therapy for lymphedema and selected comorbidities of the musculoskeletal system. In: Földi M., Földi E. (Ed.): Textbook Lymphology. 7th ed., Elsevier GmbH, 508.
- Brenke R., Siems W. (1996): Adjuvant Therapy for Lymphedema. Lymphol 20, 25-29.
- Flemming D. (2016): The technique of deep oscillation. Lymph self-help, 22-23.
- Gasbarro V., Bartoletti R., Tsolaki E., Sileno S., Agnati M., Coen M., Conti M., Bertaccini C. (2006): Ruolo dell'oscillazione profonda (Hivamat® 200) nel trattamento fisico del linfedema degli arti. La medicina estetica 30 (4), 473-478. English title: The role of deep oscillation therapy (Hivamat® 200) in the physical treatment of the lymphoedema of the limbs.
- GDL (Society of German-speaking Lymphologists) u. DGL (German Society of Lymphology) (2017): AWMF-S2k Guideline "Diagnosis and Treatment of Lymphedema" (AWMF Reg. No. 058-001).
- Jahr S, Schoppe B, Reisshauer A. Effect of treatment with low-intensity and extremely low-frequency electrostatic fields (Deep Oscillation) on breast tissue and pain in patients with secondary breast lymphoedema. J Rehabil Med. 2008 Aug;40(8):645-50. doi: 10.2340/16501977-0225. PMID: 19020698.
- J of IMAB 2016 Jul-Sep;22(3):1248-1252 Improving the quality of life through effects of treatment with low intensity, extremely low frequency electrostatic field with DEEP OSCILLATION® in patients with breast cancer with secondary lymphedema to patients treated with standard lymph equipment. Atanas Petkov1 Corresponding Autor, Yana Kashilska2, Angel Uchikov1, Dean Batzelov3,
- Jui Chu Y. (2017): HIVAMAT 200. In: Jui Chu Y. (Ed.): What Can Physical Therapy Do After Breast Cancer Surgery. CARE, 187-188. German translation: What can physical therapy do after breast cancer surgery.
- Kraus R. (2014): Intensive lymphatic drainage through deep oscillation. LYMPH & Health 2, 6-8.
- Lipiska A., Opuchlik A. (2014): Fizycoterapia w onkologii. In: ?liwi?ski Z., Siero? A. (Ed.): Wielka Fizjoterapia. Elsevier GmbH, 289-294. English title: Physical Therapy in Oncology.
- Mortimer P., Levine G. (2019): Let's Talk Lymphoedema, The Essential Guide to Everything You Need To Know
- Reisshauer A., Pögel S. (2010): Treatment of Secondary Arm Lymphodema in Breast Cancer. Gynecol. prax. 34, 489-499.
- Reißhauer A., Auler S., Bieringer S., year S. (2009): physical decongestive therapy. In: Reißhauer A., Auler S., Bieringer S., year S. (Ed.): Compendium of the lymphological compression supply. Federal School of Orthopedic Technology, 42-57.
- Seidl H. (2006): The HIVAMAT procedure in the context of decongestive therapy. In: Bringezu G., Schreiner O. (Ed.): Textbook of Entstauungstherapie. 2nd ed., Springer Medizinverlag, 245-250
- Schingale F.-J. (2006): Head, breast and genital lymphedema - a special challenge for the lymphatic therapist. vasomed 1, 30-31
- Talbot C. (2011): Lymphoedema Support Network periodical 'Lymphline', Spring Issue, Deep Oscillation for lymphoedema
- Teo I., Coulborn A., Munnock DA (2016): Use of the HIVAMAT® 200 with manual lymphatic drainage in the management of lower limb lymphoedema and lipoedema. Journal of Lymphoedema 11 (1), 49-53
- Theys S., Deltombe T., Legrand C., Hanson P. (2008): Manual Drainage with or without DEEP OSCILLATION® in Lower Extremity Oedema. J Rehabil Med Suppl 47, 62.
- Kraus R. (2014): Intensive lymphatic drainage through deep oscillation. LYMPH & Health 2, 6-8.
- Talbot C. (2011): Lymphoedema Support Network periodical 'Lymphline', Spring Issue, Deep Oscillation for lymphoedema
- Wehner H., Wehner W. (2006): Additional physiological help against lymphatic stasis, edema and pain. HIVAMAT® 200: It's hard to imagine day-to-day hospital practice. Naturopathy 4, 43-45.

