Head and Neck Lymphoedema – A Blog by Gaynor Leech LWO Community
Head and Neck Lymphoedema is probably the cancer-related Lymphoedema that until a couple months ago, I knew very little about. L-W-O Community has had members with Head and Neck Lymphoedema but recent call outs by me to talk to members with this Lymphoedema produced no results. So far in a recent poll, which ran on support group - no one ticked the box for head and neck Lymphoedema.
I found Head and Neck Lymphoedema (Secondary Lymphoedema) is one of the most difficult Lymphoedema's to write about. According to Cancer Research UK there were 12,422 cases between 2016-2018 with 4,077 deaths.
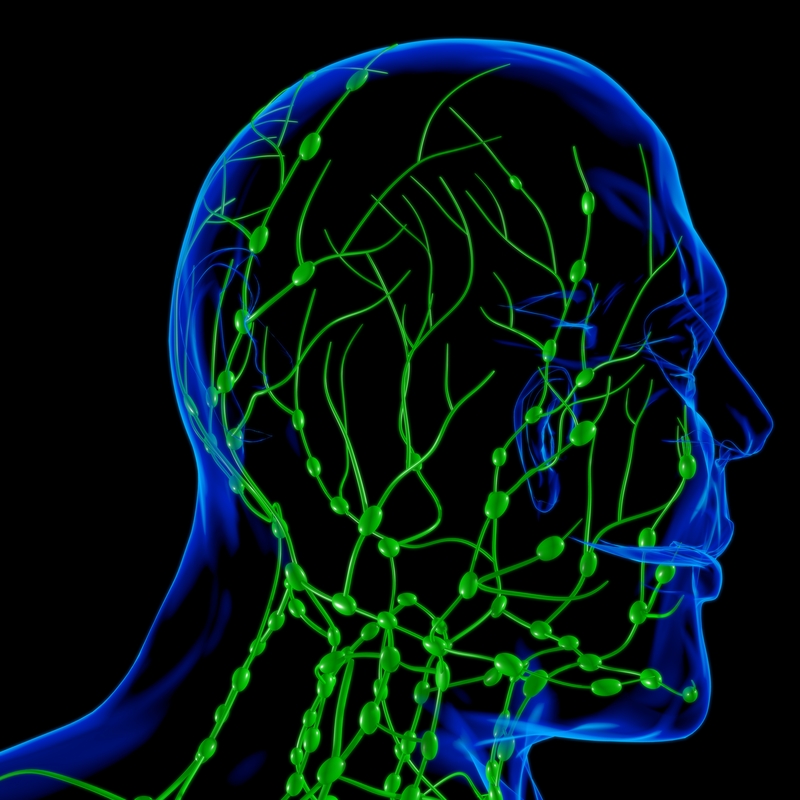
Treatment for these cancers may combine surgery, radiotherapy, chemotherapy, or cancer medication. The surgery and radiotherapy treatment to the lymph node areas can increase the risk of Lymphoedema and scar tissue. These treatments are likely to disrupt the lymph function. The swelling can develop both externally and internally. Externally the swelling will be visible in the soft tissues of the face, mouth, and neck. Internally the swelling may develop in the oral cavity, tongue, throat, and airway.
Head and Neck Lymphoedema, develops when the body is unable to transport fluid to the damaged lymphatic system because scarring from the surgery blocks lymphatic vessels in the neck or the radiotherapy treatment to the neck has damaged the lymphatic system.
Health care providers tend to concentrate on the treatment of the cancer and very often the side effects like Lymphoedema become secondary. This will also depend in the UK where you live and which services are available, whether your Lymphoedema has been recognised, assessed, and diagnosed properly.
Treatment for Lymphoedema should be part of a multi-disciplinary approach which in the case of head and neck Lymphoedema may include Speech and Language Therapists. The UK is developing a cancer pre-habilitation package of care for after diagnosis, but before cancer treatment starts. As a patient you are entitled to be consulted on every aspect of your care and a person-centred approach, which allows you to discuss treatment options, risk-reducing activities and access to Lymphoedema services.
Cancers to the head and neck are on average 3 - 5% of all cancers but imagine my surprise to learn that 90% of all patients treated for head and neck cancers will experience some degree of Lymphoedema. That is an exceptionally high figure. At the time of writing, I do not have an answer as to why being diagnosed with Lymphoedema after head and neck cancer treatment is higher, than being diagnosed with Lymphoedema from other cancers.
I do understand why our members who have this side effect after treatment would not want to talk to me about this type of Lymphoedema, or share in group how they feel because of the impact that this has on their lives.
“The impact of head and neck Lymphoedema has a serious impact on both physical and mental health. The physical side effects may include facial disfigurement due to increased swelling and this can have a devastating effect on self-esteem.
Breathing, hearing, speaking, swallowing and vision may all be affected. A person with head and neck Lymphoedema may experience a loss of identity.”
Management strategies are key and include, education, skincare, stretching and movement, both manual lymphatic drainage and simple lymphatic drainage, Kinesio taping, compression.
As with all Lymphoedema life-long self care for our members is crucial and priorities will include:
- Skincare, daily washing and moisturising
- Shaving with an electric razor and it is important for men to continue with normal shaving habits
- Antiseptic treatment of cuts or scratches to the skin
- Good oral hygiene, mouth and dental care is essential
- Nutritional Care
- Protect face and neck from sunburn
- Do not wear restrictive clothing around the neck
- Lymph Drainage
Stretching and movement are very much part of the daily routine for head and Lymphoedema. Simple facial movements like frowning, smiling, and yawning can make a significant difference to swelling and these should be part of a daily routine.


