Gaynor Leech Guest Blog - June 2022
Lymphoedema & Blood Pressure Monitoring

This is being written from a patient perspective and is just one of the many questions that come up regularly within the L-W-O Community support group. The question comes from a Breast Cancer Related Lymphoedema (BCRL) patient whose advice not to have invasive procedures to their affected limb including blood pressure readings, blood tests, injections, or IVS left her frustrated and stressed after a GP appointment.
The latest post on this topic came from one of our members who has secondary Lymphoedema in left arm, chest and back after left mastectomy and Sentinel Lymph Node Biopsy (SLNB) in November 2018. Unfortunately, in January this year our member was diagnosed again and had right mastectomy and SLNB earlier this year. This is the latest post (April 2022) from one of members after visiting her GP.
“I have been advised by the hospital that I should have BP taken on leg! GP was not happy about this and wanted to use Lymphoedema arm or newly at-risk arm, he said he did not have a cuff big enough to do leg BP.”
This is a frequent problem, not just from GP’s but practice nurses and A & E or those healthcare professionals who are not familiar with Lymphoedema. Those of us who have lived with Lymphoedema for a long time, will have been told 'under no circumstances' do we allow any invasive procedures to our affected limbs. While Lymphoedema patients often get the NICE guidelines quoted to us, if you are told, when first diagnosed with Lymphoedema that, 'any form of invasive procedure to your affected limb should be avoided' then, as a patient you are going to be extremely protective of your limb.
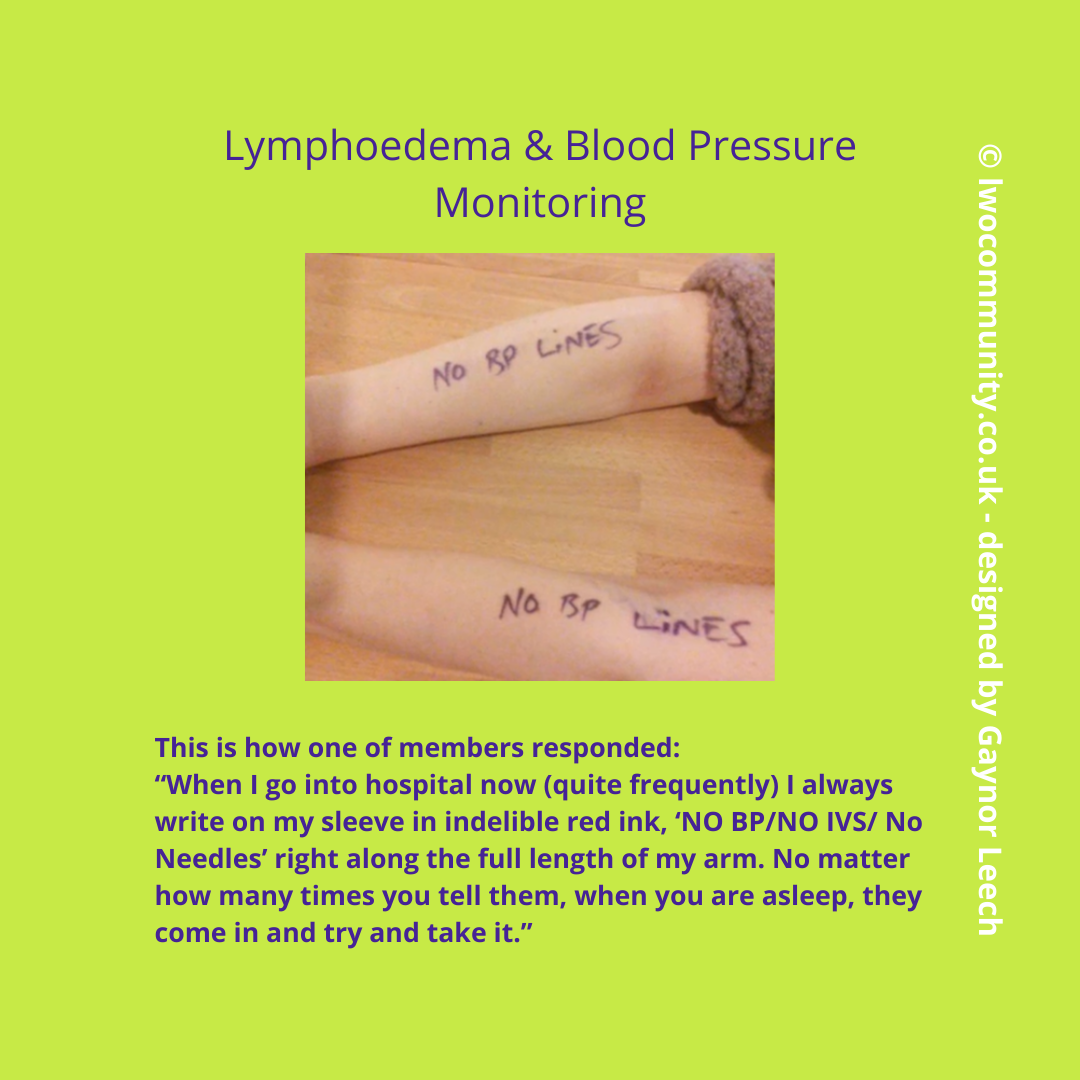
Below is a comment from one of our L-W-O Community members on their experiences with blood pressure monitoring.
There is an additional problem as more services are undertaken in pharmacies, such as blood pressure monitoring and vaccination services. Pharmacists have repeatedly told our members they can only use an arm; their training does not extend to using a thigh or the lower part of the limb. In addition to this, most Pharmacies would not have the space in the case of taking blood pressure from a lower limb for the patient to lie down.
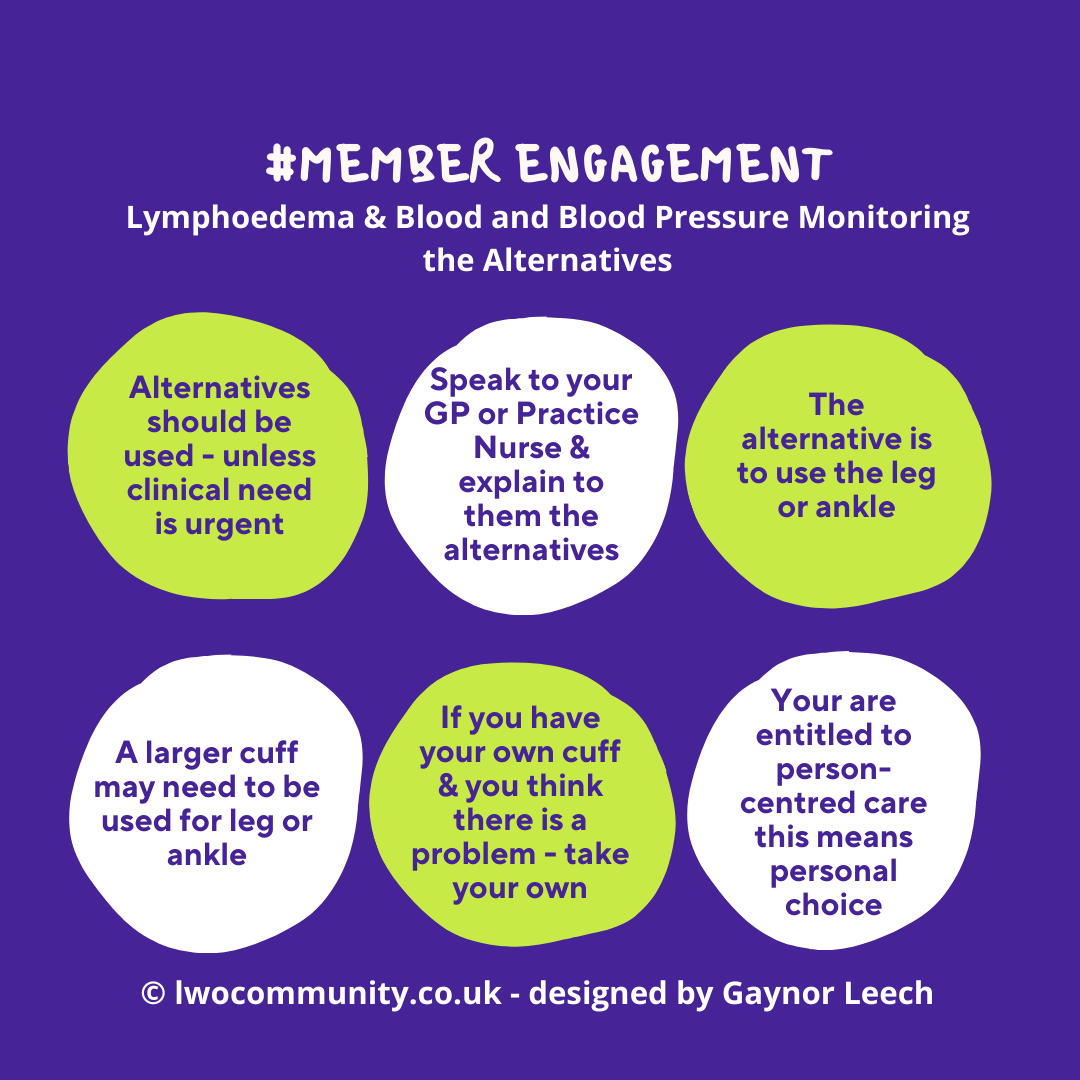
Member Engagement
This was the question I put to our members.
“This morning I am playing Devil's Advocate for an article I am writing that requires #memberengagement re the recent post on blood pressure monitoring, so let’s look at the relevant section in the guidelines. What would be your interpretation of this?”
This is the guidance from NICE:
“There is no consistent evidence of increased risk of lymphoedema associated with medical procedures (for example, blood tests, injections, intravenous medicines, and blood pressure measurement) on the treated side, and the decision to perform medical procedures using the arm on the treated side should depend on clinical need and the possibility of alternatives.”
The general response from our members was “NO, NO, NO!”
Purely from a patient view picking apart the above advice, while there may be ‘no consistent evidence’ neither I, nor our members, would take that risk unless it was a life-or-death situation. The second statement in bold is in ‘possibility of alternatives’ this is where the conflict between patient, GP’s, practice nurses, healthcare professional (HCP’s) becomes an issue because of the advice given to patients on their diagnosis therefore, the patient’s personal choice must be listened to.
On a personal level, I repeatedly inform HCPs when they are reluctant to abide by my wishes in respect of my Lymphoedema to use an alternative site that I will say…
“It is not best practice”
However, I do find most HCPs do listen and are respectful of my wishes. Every patient is entitled to person-centred care, and we do need to try and build a good relationship with those healthcare professionals we encounter.
My advice to our member, was to speak to her Breast Care Nurse (BCN) and see if she would be willing to write to the GP to explain why it is important to use the ankle/leg instead of the arm. Sadly, our member didn’t have a pleasant experience and was made to feel uncomfortable. She left the surgery, without having her blood pressure taken. This means that the health problems she was experiencing were not dealt with. This is not an isolated case amongst our members.
At this point, I would like to acknowledge the input of Karen Friett from the Lymphoedema Support Network who made several suggestions including the use of a thigh blood pressure monitor, speaking to practice nurses, giving them the time, if need be, to brush up on the techniques. Usually when taking blood pressure from the lower limbs the readings will be different and the patient would need to lie down while the readings were taken. Thank you, Karen.
Those of us who live with Lymphoedema are extremely protective of our limbs and we do understand that health-care professionals have a job to do but we both need to be able to talk to each other with an open mindedness to any alternative ways.
There is more information on Breast Cancer Related Lymphoedema on our website. Being diagnosed with cancer is hard enough to be further diagnosed with Lymphoedema and the complications it brings needs a lot more awareness, understanding and most of all, education.


xxx
EDITORIAL COMMENT
PhysioPod UK asked Sue Hansard, Lymphoedema Nurse Specialist of First Lymph Care for her thoughts on the subject of blood pressure measurements and Lymphoedema
.jpg)
'Sadly Mary, there is a paucity of research into the effect of taking blood pressure readings on a limb affected by/or at-risk of lymphoedema.
The current advice that Lymphoedema Practitioners and educators give to Lymphoedema patient groups is:
* If possible and practicable, avoid having blood pressure readings taken on your affected/at risk limb. (arm/leg)
* If possible and practicable, avoid having injections and venepuncture (blood sampling), and tattoos, on the affected/at risk limb. (arm/leg)
* If an alternative method is not possible, or due to an emergency situation, then the affected/at risk limb may need to be used.
The NHS Website advise:
'You can reduce your chances of developing skin infections by: not having injections or blood pressure readings in the affected area whenever possible'. [1]
The Lymphoedema Support Network (LSN) advise:
In this video chat on the LSN 'Ask The Experts' Professor Mortimer and Anita Wallace MBE discuss having blood tests, blood pressure readings and drips in an at risk or lymphoedema arm both confirm
'Wherever possible, avoid blood pressure measurements injections or blood samples being taken from the at risk limb’ [2]
The Royal College of Anaesthetists (RCoA) advise:
'Although there is little evidence, these procedures could potentially trigger lymphoedema on the arm on the side from which glands have been previously removed. Therefore, whenever possible, staff should use the arm on the other side. Sometimes they may mark the “at risk” arm to remind other staff not to use it. If they have to use a tourniquet on the affected limb, they will only do so for a short time. If there is no lymphoedema in the “at risk” arm, and the other arm cannot be used for whatever reason, it is reasonable to put a cannula or use a blood pressure cuff on the affected arm, especially in an emergency situation'. [3]
Royal College of Nursing (RCN) Advice
'Unless there is a medical emergency, avoid taking blood pressure measurements, injections or blood samples from the ”at risk” limb as this may lead to infection and/or the onset of lymphoedema. This is also the case in people who already have lymphoedema. For women who have had bi-lateral surgery or radiotherapy, blood samples may be obtained from other areas of the body, such as the feet or legs (RCoA, 2008)' [4]
Research Evidence
Asdourian m. et al concluded 'Blood pressure readings, blood draws, injections, and number or duration of flights were not significantly associated with increases in arm volume' [5]
Cemal, Yeliz et al. conducted a detailed literature review, looking at a variety of recommendations which were common within Lymphoedema management [6] . Avoidance of Blood Pressure readings was challenged by Greene et al [7] with the hypothesis that 'because patients wear compression the inflation of a blood pressure cuff would not be harmful.' However, this seems to overlook the fact that compression exerted by garments is graduated throughout the length of the limb, whereas a blood pressure cuff exerts high pressures (albeit for a few minutes only), over an 8cm section of the upper arm. And it did not consider the continuous inflation/deflation during surgical procedures.
Assmus and Staub reported that short applications of a tourniquet for specific hand surgery (10 minutes) , caused no adverse effect. [8]
'But it happened to me'
Yes there are incidences where someone attributes the onset of lymphoedema to a blood pressure reading being taken. They are rare though. In fact, in my 20+ yrs experience, I have probably only come across 2/3 whose lymphoedema became apparent in this way. What we don’t know is whether these had latent, as yet undiagnosed, mild L/O at the time their BP was taken. Where someone had BP taken and existing diagnosed L/O became worse , that perhaps does point to pressure from the cuff being an aggravating factor. We do need to bear in mind that there are times when other medical conditions need careful and accurate assessment , monitoring and treatment and there may be occasions when the affected/at risk limb needs to be used because the alternatives are not suitable, or possible.'
References
- NHS website Prevention-Lymphoedema
- Ask The Expert, Professor Peter Mortimer and Anita Wallace discuss blood pressure and needles in the 'at risk' arm, (2021)
- 'Information for patients at risk of lymphoedema undergoing anaesthesia and surgery' Royal College of Anaesthetists (RCoA) Factsheet (2018)
- 'Reducing the risk of upper limb lymphoedema - Guidance for nurses in acute and community settings' Royal College of Nursing, Publication code 004 138, ISBN 978-1-906633-83-7 (2011)
- Cemal, Yeliz et al. “Preventative measures for lymphedema: separating fact from fiction.” Journal of the American College of Surgeons vol. 213,4 (2011): 543-51. doi:10.1016/j.jamcollsurg.2011.07.001
- Association Between Precautionary Behaviors and Breast Cancer–Related Lymphedema in Patients Undergoing Bilateral Surgery
Maria S. Asdourian, Meyha N. Swaroop, Hoda E. Sayegh, Cheryl L. Brunelle, Amir I. Mina, Hui Zheng, Melissa N. Skolny, and Alphonse G. Taghian
Journal of Clinical Oncology 2017 35:35, 3934-3941 - Greene AK, Borud L, Slavin SA. Blood pressure monitoring and venipuncture in the lymphedematous extremity. Plast Reconstr Surg. 2005 Dec;116(7):2058–2059
- Assmus H, Staub F. Postmastectomy lymphedema and carpal tunnel syndrome. Surgical considerations and advice for patients. Handchir Mikrochir Plast Chir. 2004 Aug;36(4):237–240.

