Ever Thought of Specialising in Lymphoedema? Sue Hansard, Lymphoedema Nurse Specialist
"Early one Saturday morning in 1996, I was putting my uniform on for the first time in 13 years. It was to be my first shift as a volunteer nurse in a local hospice. My first tentative step to returning to the profession I had longed to be part of since the age of seven. My stomach was turning somersaults, my mouth dry and I felt incredibly out of my comfort zone. The welcome was warm, with undertones of bemused curiosity:

“Why was I volunteering?”
“Why didn’t I just join the ‘Bank’?”
“Why had I even taken 13 years out to bring up my family?”
SEEDS SOWN

When I was about 5/6 years old, my Dad needed daily visits from a District Nurse. I had no idea why he was ‘out of bounds’, in bed and resting but Nurse Kissock had a kind motherly face and nipped briskly up the stairs, carrying her leather bag to minister to Dad with a calm reassuring confidence.

I was in awe...... and I wanted a uniform and bag like that!
My interest was duly noted and that year Santa brought me a wonderful nurse’s uniform, with ‘fob’ watch, apron and ‘hat’,(No bag though, which was disappointing) However, I discovered our medical box - an old biscuit tin, with bandages, dressings, scissors and ointments. I spent many Saturday afternoons ‘bandaging’ my Dad’s leg while he cat-napped and I distinctly remember using biro to draw’ veins’ on my favourite doll and practising injections on her using a darning needle.
At primary school, I encountered more nurses. The vaccination nurses, giving us ‘polio’ sugar cubes. The Nit Nurse, who checked us all for lice. Then aged 10 years, I discovered that if I offered to escort younger children when they needed to visit the Child Welfare Clinic, near school, I would miss catechism lessons! So, I had regular contact with the nurse, as she dabbed gentian violet on minor skin conditions and applied dressings over oozing cuts and scrapes. It all fascinated me.
I started reading our family medical encyclopaedia, intrigued and puzzled by the illustrations of a naked man and woman with certain parts of their anatomy covered up!
Growing up, I often accompanied my Mum as she visited and helped the elderly and lonely and I often ran errands or did shopping for them. At 14 years, I joined a group of First Aiders and as a Sixth former, I volunteered at ‘Jimmy’s’ (St James’s Hospital, Leeds) helping elderly patients at meal times.
I had already decided that I would apply to train as a nurse, but also wanted to do something more academic. Done consecutively would take 6 years, but in 1978, Polytechnics and some Universities were offering something new: Nursing Degrees. These combined academic study with practical training and would lead to a Nurse qualification plus degree. I applied and became an undergraduate at Newcastle Polytechnic. It would prove to be an intensive challenging and rewarding 4 years.
The course was really well designed, directly linking each term’s academic learning (anatomy and physiology, psychology, social policy and nursing theory) with the 8-week clinical placements.
And unlike traditional nurse training at the time, and probably also today, the course followed a logical pathway from birth, through childhood, to adulthood. It flowed so well. In our fourth and final year, we had to write a 20,000-30,000-word Dissertation while working in extended clinical placements, including elective choices. I chose gynaecology and geriatrics and wrote a dissertation on the effect of nutritional status in cancer related cachexia. Little did I know that, years later I would specialise in cancer and palliative care.
As students, we had an 8-week Summer break during which I returned home to work as an Auxiliary nurse on a geriatric ward. The staff were supportive and enabled me to gain and hone many practical skills including injections and my confidence grew.
BECOMING A REAL NURSE

Graduation - November 1982 - Newcastle Upon Tyne, City Hall
In June 1982, I tentatively scanned the Pass List, posted on the Health Studies noticeboard . To have failed on my dissertation would have meant I would also have failed as a nurse.
No Degree, no State Registration.
So, it was a huge relief to see my name there and a strange feeling too because it marked the culmination of 4 year’s hard work. It would take several months for our registration to be finalised and as students, we were not NHS employees, so had no job guarantees. I had applied for every job advertised in Barrow In Furness! Why? Because that is where I would be starting my married life.
NEW BEGINNINGS
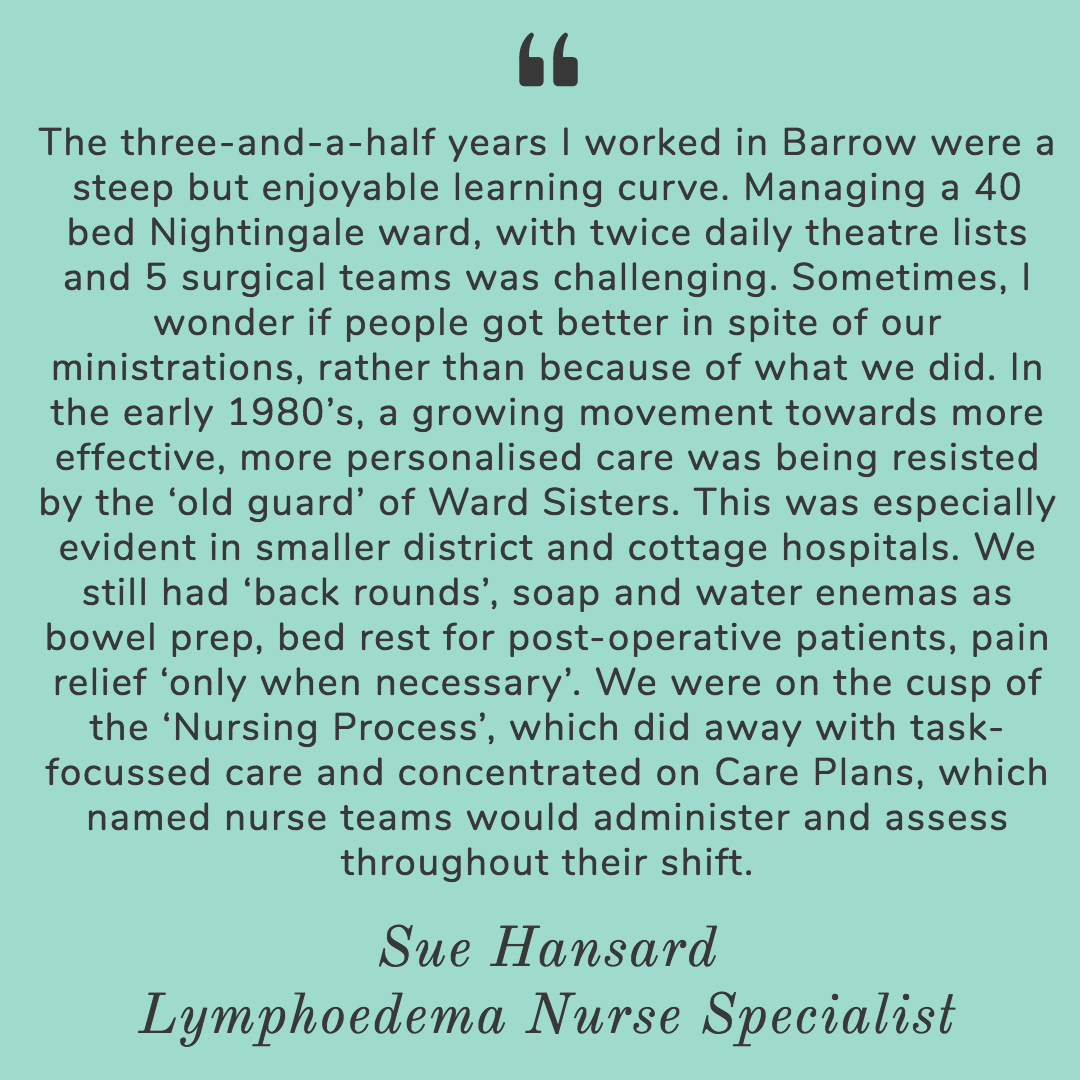
For the first month as a Staff Nurse on a female surgical and orthopaedic ward, the ward sister ignored me. Word had got around that I was a ‘degree nurse’. Sister, a cadet nurse at 16 years, who had worked her way up the ranks, had no time for new-fangled qualifications. To cap it all, my appointment meant that one of their eight local trainees did not get a post at the hospital. She was determined I would never come up to scratch.
I knew Sister had accepted me, when she asked me to join her in the ward kitchen for a cup of tea while she had a sneaky cigarette and the patients were tucking into their breakfasts!
When I became pregnant with my son, I left nursing. We did not have family nearby, nurseries were few and far between and I wanted us to be fully involved as parents. When I returned to show off my baby to that same, strict and slightly terrifying ward sister, she presented me with a beautiful, fine hand-made ‘angel top’ for him. Apparently she had never done so for anyone else. I think I must have proved myself to her!
FAMILY TIME
In the event I was out of nursing for 13 years, focussed on bringing up our two children and becoming immersed in all things educational, from mother and toddler groups, Volunteer teacher’s help, PTA Treasurer, and of course helping our son and daughter with homework, attending concerts, parents evening etc, etc.
But I always kept an interest in all things nursing and medical, and read anything relating to Hospice care.
When we moved to the Midlands and I discovered there was a local hospice I applied to be a volunteer, thinking I would help serving meals or washing up. My first interview in 15 years was nerve-wracking. Matron quickly noted that I had been a nurse and decided that I would therefore be a Volunteer Nurse on the In-Patient unit. After my first duty, I realised I had found my ‘niche’, so I completed retraining, gained a palliative Care qualification and joined the night team working a twilight shift (9pm-Midnight) which dovetailed nicely with family life.
LIGHT BULB MOMENT
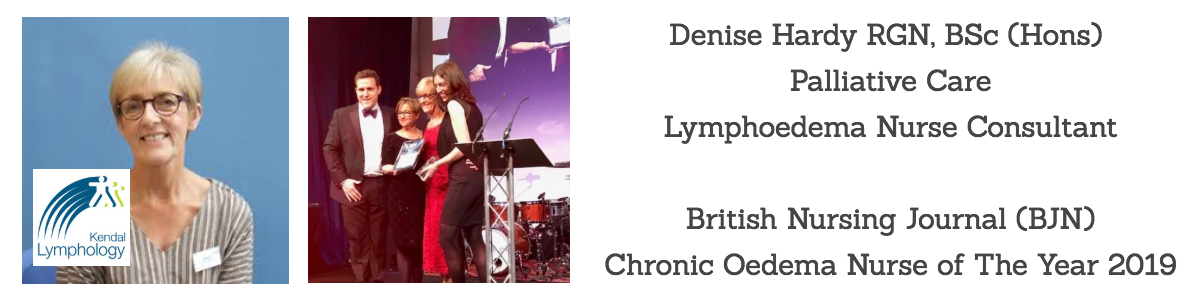
The Hospice in the Midlands had an excellent programme of in-house training and I attended a study day about Lymphoedema taught by Denise Hardy RGN, BSc (Hons) Palliative Care Lymphoedema Nurse Consultant, I was hooked. Denise invited to me train up as a Bank Nurse at the Lymphoedema Clinic she had set up there and I jumped at the opportunity. By 1998, I was working three twilight shifts a week and some half days in Denise's Lymphoedema clinic.
WHAT IS LYMPHOEDEMA?
"Lymphoedema is a swelling that develops as a result of an impaired lymphatic system. This may be as a result of the lymphatic system not developing properly or through damage or trauma. It can affect any part of the body but is most commonly seen in an arm or a leg. Although thought to be relatively uncommon, recent research suggests that 6 in every 1,000 people in the UK may be affected by this condition". Read more on LSN..
LYMPHOEDEMA TRAINING
By the time the clinic moved into a new purpose-built facility, I was working weekly in the clinic, gaining as much practical experience as I could. But I needed to learn Manual Lymphatic Drainage massage (MLD) and more advanced skills in Lymphoedema Management. I received funding to attend a new course: L.D.I. The Alan Hudson Technique, taught at Regents College, London by an inspiring teacher: Liz Fletcher.
The course was on weekends and spread over nine months, in three stages with course work and exams. I loved the learning environment and the practical training and though challenging has provided a firm foundation for my approach to MLD ever since. I still use the techniques for head and neck drainage which she taught me, adding in Deep Oscillation now to achieve excellent results.
Eventually I took on a permanent role within the clinic, always keen to learn more from other practitioners and through study days and Conferences. I worked in the Lymphoedema at LOROS, Leicestershire, for a secondment, covering study leave. Again, a great opportunity to expand my knowledge and experience in this specialism. Both services treated all types of Lymphoedema, so there was a huge variety in presentations, and patient experiences.
Over the years I gained qualifications in the Leduc method of MLD and more recently, the FG-MLD® Fill & Flush technique taught by Jane Wigg, another inspiring teacher. This is the technique I now update every two years and which is taught at The Lymphoedema Training Academy and was pioneered by J.P. Belgrado.
INDEPENDENCE
In 2003, I qualified as a Lymphoedema MLD Practitioner and also studied Indian Head Massage. I decided to launch my independent therapy business, working Saturdays at a Complementary therapy centre and evenings at home, alongside weekdays in the Lymphoedema clinic. It quickly took off. I enjoyed the contrast of working in a less ‘clinical’ environment and making independent decisions and advice. This in turn, helped me in my clinical decision making. Lymphoedema is one of a few specialisms where a service is often led, (even instigated) by a nurse, physiotherapist or occupational therapist, rather than a doctor. So, it is vital that we have in depth knowledge and understanding: the buck stops with us!
.jpg)
Teaching Nurses in Bulgaria, for charity: Krasifaid
I attended ‘Holistic Therapy’ events, gave talks and demo’s to local groups: Breast Friends, Carers Groups, Church groups. I created my own patient guides and advice sheets and I found that now I was treating people who did not have Lymphoedema, but who benefited from MLD for other reasons.
NEW CHALLENGES
In 2016 I left my job of 18 years and joined the Lymphoedema Service at Mary Ann Evans Hospice, Nuneaton. Led by Kay Hill, who had established the service 10 years previously, this small clinic treated adults with cancer related Lymphoedema. Again, I was blessed to work with an inspiring team lead who was not afraid to use innovative technology and approaches to care.
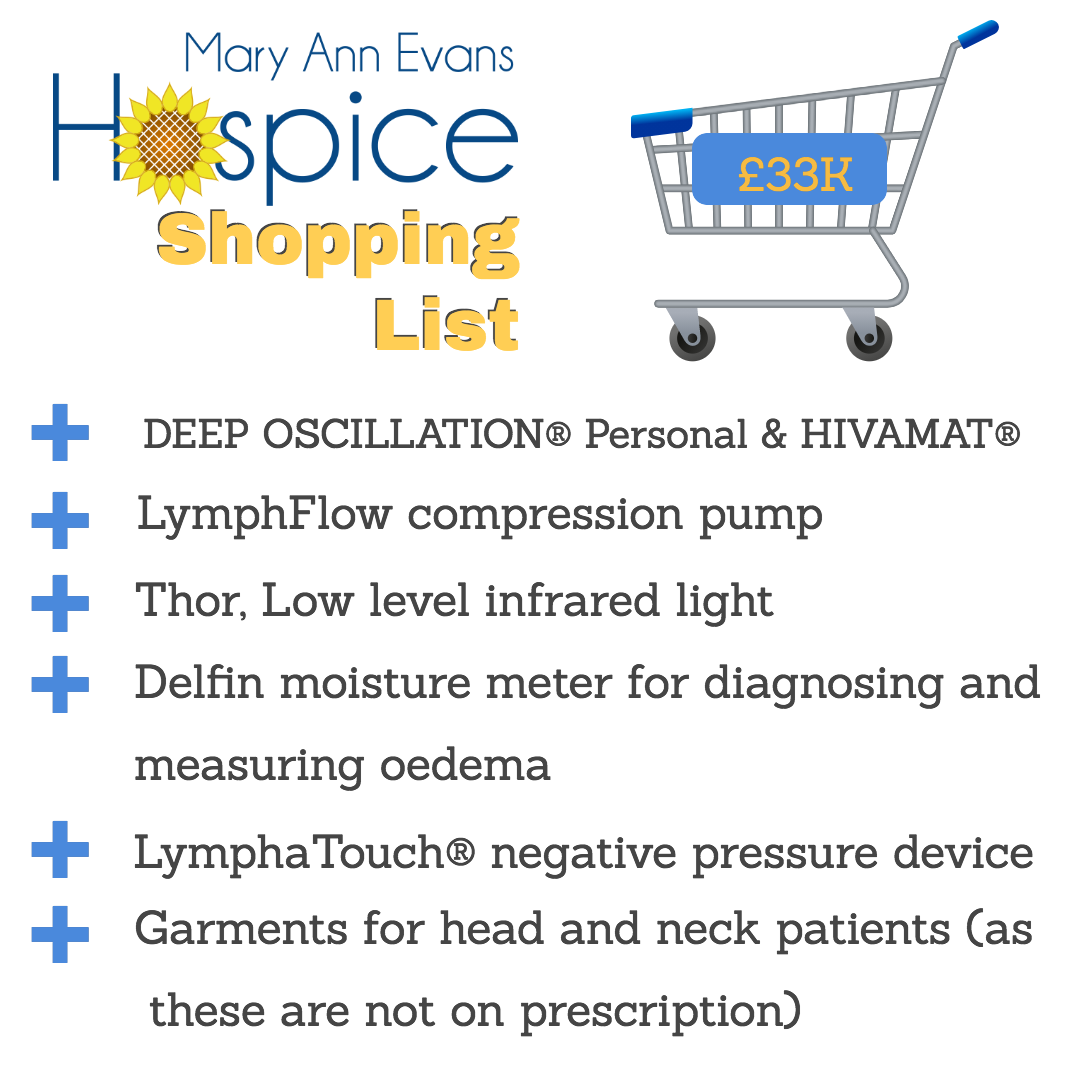
When Kay was promoted, I became team lead and the same week, we became the recipients of a £33, 000 donation from the Mayoral fundraising Appeal. The money was for equipment which would enhance care for local people diagnosed with this life-long condition.
MY £33,000 SHOPPING LIST

Picture above: Bill and Sheila, who achieved awesome fundraising Lord Mayor and Lady Mayoress of Nuneaton and Bedworth with the Mary Ann Evans Hospice Lymphoedema Team. They raised £33,000 for Mary Ann Evans Hospice Lymphoedema Service. They made the team's dreams for specialist, innovative equipment to enhance our treatments, come true......"
AS a team, we discussed what would be most beneficial for our patients and what items the clinic would be able to use the most. We had seen many different technologies at recent conferences and already had some specialist devices in clinic. We considered some of our more complex cases: was there something that could specifically improve our treatment for them?
A few months previously a gentleman with complex Head and neck Lymphoedema was referred to the clinic. His condition was proving very difficult to treat. I liaised with other Lymphoedema specialists who suggested Deep Oscillation but I knew our small Hospice did not have funds to buy this equipment, so I contacted Mary at PhysioPod, to enquire about loaning a device. Instead Mary and Julie offered to visit clinic, meet the patient (with consent) and demonstrate the equipment. Mr A, keen to try anything, agreed and thoroughly enjoyed the treatment that Julie gave, and we could see a subtle change in his oedema. Better still they very kindly loaned us equipment to trial in clinic, and also for Mr A to use at home between appointments.
We quickly became adept at using Deep Oscillation, saw speedy results and found that all patients liked having the treatment. So, top of the list: DEEP OSCILLATION THERAPY..
2020 COVID PANDEMIC- ALL CHANGE
.jpg)
The first national lockdown in March 2020 was a strange and uncertain time for everyone and it marked another nursing milestone for me: I retired from MaryAnn Evans Hospice. I had planned this, so that I would be able to see my small grandsons more often, while also continuing my independent work, which was to include consultancy work, professional mentoring and training.
But my last day was spent at home, ‘confined to barracks’ and in the following months any prospect of seeing my family became a longed-for hope.
Quickly ‘ZOOM’ became my friend: Family chats, professional meetings, webinars and courses . I embraced the opportunity to learn including Covid-safety certification. While developing my own Covid policies and procedures. I also started to provide remote support for current clients and anyone needing help and advice with Lymphoedema/lLipoedema.
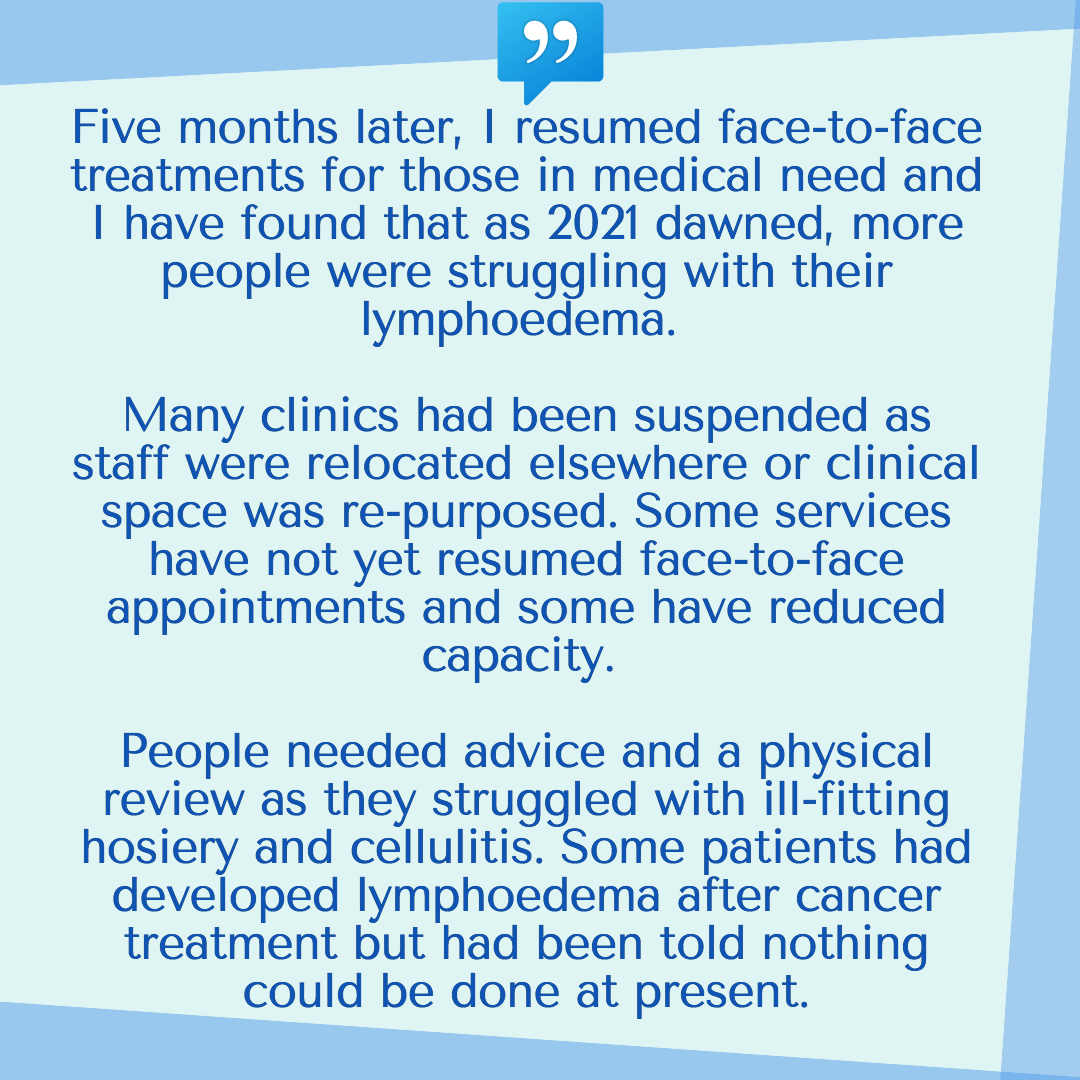
Initiating treatment for these clients, including teaching many self-management strategies was a vital part of their recovery. Hosiery and equipment companies were invaluable to me and my patients as a source of advice and support. Physiquipe, kindly loaned me LymphaTouch to help specific clients, Juzo, Thuasne and Medi provided garments for more complex patients and I was able to keep up to date with new developments and products via the reps.
So here we are 14 months later, eagerly anticipating the lifting of restrictions by June as our country’s vaccination roll out continues apace.
I continue to be busy with longstanding clients and regular new self-referrals: adults of all ages and all types of lymphoedema, lipoedema , other medical conditions, post cosmetic surgery and those who simply need to relax. I am a hungry life-long-learner so there are plenty of courses, and virtual conferences in my diary. And while the mentoring and consultancy work has been halted by Covid, I am still engaged in writing and peer review work.
Looking back: I could never have imagined how my nursing career would have panned out. I have always felt so privileged to be involved in the care of all of my patients. To help someone regain physical and psychological health and to provide encouragement and support is so rewarding. Working in Lymphoedema as a specialism has given me so much. I found my ‘niche’, but I will never know enough about it and will never stop wanting to learn and understand more, for the benefit of my patients.
WHY WORK IN LYMPHOEDEMA?
Just as Lymphoedema and the lymphatic system are dynamic, so is working in this specialist field. Treatment choices have improved considerably and our knowledge and understanding of the causes of lymphatic disease is now underpinned by an expanding wealth of research and Best Practice.
Research has led to some huge shifts in our thinking and approaches to treating lymphoedema. It has produced innovative technology used in all aspects of lymphoedema treatments and management, from a smorgasbord of compression hosiery, to equipment which improves lymph flow, measures fluid content or identifies an individual’s unique drainage pathways enabling accurate treatment planning or restorative surgery.
But my own journey into this wonderful specialism isn’t a road map for everyone; there are many, so many possible routes.
In the UK Lymphoedema Care is predominantly nurse led, predominantly female and currently weighted towards the 50-60-year age range. We have many amazing clinical specialists around the UK who have been working in the specialism since the early 1990’s- our innovators and many are my influencers and teachers. But we really do need more HCP’s to come into the specialism, to bring a new energy and a new hunger for knowledge and a better future for Lymphoedema provision in the UK.

USEFUL LINKS:
Free Webinars/Online Courses
Nursing Times - The Lymphatic System
BMJ Chronic Oedema and Lymphoedema
Manual Lymphatic Drainage and Lymphoedema Training
Dr Vodder with Deborah Berry Dr Vodder with MLD Training
Lymphoedema Societies/Forums/Support Networks and Community
The British Lymphology Society
Higher-level qualifications in Lymphoedema
University of Glasgow
Post Graduate Taught
Advanced Lymphoedema Management PgCert
University of Wolverhampton
Specialist Assessment and Management of Complex Lymphoedema

